Augmentation of the Facial Skeleton
Why is most augmentation of the facial skeleton done with alloplastic implants instead of autogenous bone? Unlike alloplastic materials, autogenous bone has the potential to be revascularized and then assimilated into the facial skeleton. In time, it could be biologically indistinguishable from the adjacent native skeleton. These attributes make it ideal and the only material available to reliably reconstruct segmental load-bearing defects of the facial skeleton. However, when used as an onlay graft to augment the contours of the facial skeleton, revascularization provides access for osteoclastic activity, graft resorption, and hence unreliable augmentation. Use of autogenous bone also requires a donor site, which may be unsightly or painful. Finally, use of autogenous bone as an implant material is more time consuming and therefore more expensive. Alloplastic implants do not change their shape with time and do not require a donor site.
2 .  How does an implant’s surface characteristics affect the host’s response to the implant?  The host responds to an alloplastic implant by forming a fibrous capsule around the implant. This is the body’s way of isolating the implant from the host. The implant’s surface characteristics impact the nature of this process. Smooth implants (e.g., solid silicone) result in the formation of thick, smooth-walled capsules. Porous implants (e.g., polytetrafluoroethylene [Gore-Tex], porous polyethylene [Medpor]) allow varying degrees of soft tissue ingrowth, which results in a less dense capsule.
Animal studies have demonstrated that implant pore sizes greater than 100 microns encourage tissue ingrowth. Pore sizes less than 100 microns limit tissue ingrowth, whereas materials with large pore sizes (>300 microns) have drawbacks associated with material breakdown. Clinical observation has shown that porous implants, as a result of fibrous tissue ingrowth, have less tendency to erode underlying bone, to migrate due to soft tissue mechanical forces, and, perhaps, to be less susceptible to infection when challenged with inoculums of bacteria.
3 .  What alloplastic implant materials are most commonly used to augment the facial skeleton?     • Silicone rubber, polytetrafluoroethylene (Gore-Tex, W.L. Gore, Flagstaff, AZ)   • Porous polyethylene (Medpor, Porex, Fairborn, GA)   • Polymethylmethacrylate (polyhydroxyethyl methacrylate HTR [hard tissue replacement], Walter Lorenz Surgical, Inc., Jacksonville, FL)
Silicone rubber is the material most commonly used. Silicone has the following advantages: it can be sterilized by steam or irradiation, it can be carved with either scissors or a scalpel, and it can be stabilized with a screw or a suture. Because it is smooth, it can be removed quite easily. Disadvantages include the tendency to cause resorption of bone underlying it, the potential to migrate if not fixed, and the potential for its fibrous capsule to be visible when placed under a thin soft tissue cover.
Gore-Tex has a non adherent surface that is very flexible. Implants are available for both subdermal and subperiosteal placement. Preformed implants are made with a pore size between 10 and 30 microns, which allows for some soft tissue ingrowth. However, it is smooth enough to be maneuvered easily through soft tissues. This material can be fixed to underlying structures with sutures or screws.
Medpor is firmer than polytetrafluoroethylene and has a porosity between 125 and 250 microns, which allows more extensive fibrous tissue ingrowth than does Gore-Tex. The advantages of porous polyethylene include its tendency to allow extensive soft tissue ingrowth, thereby lessening its tendency to migrate and to erode underlying bone. Its firm consistency allows it to be easily fixed with screws and contoured with a scalpel or power equipment without fragmenting. However, its porosity causes soft tissue to adhere to it, making placement more difficult and requiring larger pockets to be made than with smoother implants. The soft tissue ingrowth also makes implant removal more difficult than with smooth surface implants. HTR is porous, allowing some tissue ingrowth, but is inflexible.
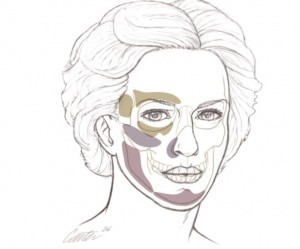
4 .  What areas of the face are most often augmented with implants?  The chin and cheekbones are the most common sites for alloplastic skeletal augmentation. Chin implants are the most frequently used alloplastic implants in facial aesthetic surgery. Malar implants are the second most frequently used alloplastic implant. Implants are available to augment all areas of the facial skeleton, including the orbital rims, the pyriform aperture, and the mandible ( Fig. 86-1  ).
5 .  What surgical approaches are used for placement of malar implants?  Malar implants are placed through both extraoral and intraoral approaches. Extraoral approaches may use eyelid, preauricular, or transcoronal incisions. Eyelid approaches are used by some when malar augmentation is combined with lower lid blepharoplasty. This approach allows excellent visualization of the zygoma and precise implant placement. However, lid malposition is not an uncommon sequela due to lid scarring and implant-induced capsular contracture. The preauricular approach can be used when malar augmentation is combined with a face lift. Transcoronal placement of malar implants can be used when malar augmentation is combined with forehead lift or subperiosteal face lift.
The intraoral approach is preferred by most surgeons. Although this approach risks bacterial contamination of the implant by organisms from the mouth, infection rates are low. Advantages of the intraoral approach include excellent visualization, ease and rapidity of placement, and no visible scar.
6 .  What is the most common complication after placement of a malar implant?  Malposition is the most common complication after malar implant surgery. This may result from inadequate exposure of the area to be augmented or failure to immobilize the implant. Sensory changes due to impingement of the implant on the infraorbital nerve are not uncommon.
7 .  What are the advantages of wide subperiosteal exposure of the skeletal area to be augmented?  Alloplastic implants used to augment the contours of the facial skeleton are placed in the subperiosteal plane. Wide subperiosteal exposure of the area to be augmented has several advantages. It allows accurate identification of the area to be augmented; of important adjacent structures, such as the infraorbital nerve, thereby preventing their iatrogenic damage; and of landmarks for orientation and, hence, symmetric implant positioning. Wide exposure also allows easy access for immobilization of the implant by sutures or screws. The resultant soft tissue mobilization allows tension-free closure of the access incision. Implants placed in large subperiosteal pockets must be immobilized to prevent their postoperative movement.
Figure 86-1 .  Areas of the facial skeleton augmented with alloplastic implants.
This technique differs significantly from the traditional approach in which dissection of only the area to be augmented was advocated. The resultant small pocket was intended to prevent postoperative implant migration. A limited dissection is possible for placement of smooth surfaced implants but is not possible for placement of porous implants to which soft tissues tend to adhere (e.g., Velcro), making placement difficult.
8 .  Why should I consider fixing an implant to the skeleton with a screw? S crew fixation of the implant to the skeleton provides both practical and theoretical advantages. Screw fixation prevents movement of the implant, which adds precision as well as early and late predictability to the result. Theoretically, elimination of implant motion should hasten fibrous incorporation while minimizing capsule formation and underlying bone resorption. By applying the implant to the skeleton, screw fixation eliminates any gaps between the implant and the recipient bed. Gaps are potential sites for hematoma or seroma accumulation. Gaps also result in an effective increase in augmentation. For example, a 2-mm gap between the posterior surface of a 5–mm implant would produce an augmentation equivalent to a 7-mm implant whose posterior surface was applied directly to the anterior surface of the skeleton. Screw immobilization of the implant allows in-place contouring of the implant at the recipient site. This final adjustment can be performed with a scalpel, rasp, or high-speed burr, depending on the material properties of the implant.
9 .  What is considered an ideal chin projection relative to the lips? Suggested ideal relationships between the chin and the lips based on normative cephalometric data by different authors are in consensus that the chin shoulder should rest slightly posterior to the lower lip and the lower lip posterior to the upper lip.
10 .  How does the inclination of the labiomental angle impact chin augmentation?  The inclination of the labiomental angle must be evaluated when considering an increase in the sagittal projection of the chin. There is a considerable variability in this inclination. In general, the inclination is more acute in men (113° ± 21°) than it is in women (121° ± 14°). When the angle is already acute, chin augmentation will make it more acute, thereby deepening the labiomental angle. Such deepening usually is dysesthetic. In certain patients with retrognathia the upper central incisors abut on the lower lip, thrusting it forward and creating a deep sulcus. These patients are better served with repositioning of the entire mandible by sagittal split osteotomy.
11 .  What is the soft tissue response to augmentation of the chin? Objective analyses showed that the soft tissue to hard tissue changes in patients undergoing alloplastic augmentation of the chin averaged between 77.7% and 90%. Variations in the soft tissue response would be anticipated because of the variability in the thickness of the chin soft tissue envelope. The thicker the overlying soft tissue envelope, the less its surface response to the underlying skeletal augmentation. The thickness in the soft tissue envelope overlying the chin varies within the individual and between individuals for any given area, and it usually is thicker in males than in females.
12 .  What muscle is most frequently injured during chin implant surgery?  The mentalis is the most frequently damaged muscle during chin surgery, usually associated with the intraoral approach for implant placement. The mentalis muscle is an elevator of the central lower lip. It arises from the mandible at the level of the root of the lower lateral incisor and therefore defines the inferior limits of the sulcus intraorally. It fans inferiorly as a truncated cone whose base inserts on the skin and therefore dimples the skin when elevating and protruding the lower lip. If it is divided and improperly reapproximated or stripped from its origin and allowed to descend to a more inferior position, the result is inferior malposition of the lower lip with increased lower incisor show and deepening of the sulcus as well as inferior displacement of the chin pad. Use of a submental approach usually avoids injury to the mentalis muscle.
13 .  How would you treat a patient who complains that the silicone chin implant placed several years ago is too large and asymmetric?  Revision surgery requires implant removal and replacement with an appropriately sized, shaped, and positioned implant. An advancement sliding genioplasty is an alternative approach to limit capsule-related soft tissue distortion. Removal of a smooth surfaced implant often reveals a distorted soft tissue envelope. The distortion will worsen with time due to ongoing soft tissue contraction forces. This distortion can be lessened if the soft tissue envelope is redraped over another implant or advanced skeletal segment.
14 .  Can fat grafts substitute for alloplastic implants to augment the facial skeleton?  Because the ultimate expression of skeletal or soft tissue structure is reflected on the skin’s surface, some surgeons have used this as a justification for the equivalence and interchangeability of soft and hard tissue augmentation. For example, malar skeletal implants are used to restore cheek fullness, whereas fat grafts are used to create malar prominence. Up to a millimeter or so, the visual effect of either augmentation modality may be equivalent depending on the thickness of the overlying soft tissue envelope. However, beyond a minimal augmentation, the visual effects of these modalities are markedly different. This is easily conceptualized when envisioning large augmentations. A large implant placed on the malar bone will make the cheek project more, making the face appear more defined, angular, and, therefore, thinner and more skeletal. Implanting fat into the cheeks will also make the cheek project more; however, the face will appear increasingly round and, therefore, less defined and less angular.
15 .  A patient has a large nose and weak chin. In what order should rhinoplasty and chin augmentation with an implant be performed?  Facial balance and harmony are important concepts in aesthetic surgery. Underdeveloped areas may exaggerate other areas of disproportion (e.g., a small chin makes the nose appear larger). Bringing this area of underdevelopment to normal dimensions with an implant changes the balance of the face and makes the nose appear smaller. For this reason, chin augmentation should be performed before rhinoplasty. After chin augmentation, less extensive nasal reduction is required to create facial balance and harmony.
16 .  What are common complications after placement of alloplastic facial implants?  The most common complications are implant malposition and sensory nerve disturbance. Hematoma, infection, extrusion, and facial muscle weakness occur less commonly. Most complications are related to postoperative hematoma that causes wound healing problems and infection. The incidence of infection, extrusion, or hematoma has been found to be less than 1% in several series.
BIBLIOGRAPHY
1. Rubin    JP  ,   Yaremchuk    MJ   :  Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: A comprehensive review of the literature .  Plast Reconstr Surg    100 : 1336 – 1353 ,  1997 .
2. Terino    EO   :  Alloplastic facial contouring by zonal principles of skeletal anatomy .  Clin Plast Surg    19 : 487 – 510 ,  1992 .
3. Wilkinson    TS   :  Complications in aesthetic malar augmentation .  Plast Reconstr Surg    71 : 643 – 649 ,  1983 .
4. Yaremchuk    MJ   :  Infraorbital rim augmentation .  Plast Reconstr Surg    107 : 1585 – 1592 ,  2001 .
5. Yaremchuk    MJ   :  Mandibular augmentation .  Plast Reconstr Surg    106 : 697 – 706 ,  2000 .
6. Yaremchuk    MJ   :  Facial skeletal reconstruction using porous polyethylene implants .  Plast Reconstr Surg    111 : 1818 – 1827 ,  2003 .
7. Yaremchuk    MJ   :  Improving aesthetic outcomes after alloplastic chin augmentation .  Plast Reconstr Surg    112 : 1422 – 1432 ,  2003 .
8. Yaremchuk    MJ   :  Making concave faces convex .  Aesthetic Plast Surg    29 :  141 – 148 ,  2005 .
9. Yaremchuk    MJ   :  Atlas of Facial Implants .  Philadelphia ,  Elsevier-Saunders, Philadelphia ,  2006 .
10. Zide    BM  ,   Pfeifer    TM  ,   Longaker    MT   :  Chin surgery: I. Augmentation—The allures and the alerts .  Plast Reconstr Surg    104 : 1843 – 1853 ,  1999 .

Leave Comments
You must be logged in to post a comment.