Clinical Experience and Example
DISCUSSION
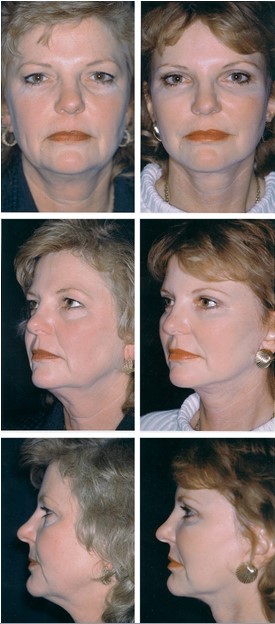
The attributes of the youthful face can be summarized as brows with an apex lateral slant, lower lids that are short, eyes that are narrow, cheeks that are full, and necks that are well defined. The combination of two major procedures, i.e., the subperiosteal brow and midface lift and a full-thickness skin and subcutaneous lower face lift, allows the surgeon to restore these youthful attributes with minimal iatrogenic sequelae. Iatrogenic sequelae include not only morbidity due to complications, such as facial nerve damage, but also the creation of “looks†that exist only after cosmetic surgery, e.g., the lateral sweep,5 the elevated and wid- ened medial brow,6,7 the distorted palpebral fissure,8,9 and the overoperated neck.10
Several conceptual and technical aspects  of this approach to total facial rejuvenation are at variance from current conventional techniques. These include the open coronal approach to the brow, the minimal manipulation of forehead musculature, the limited periorbital dissection and manipulation during  the midface lift, and lower face dissection directly on the SMAS and platysma with resultant full- thickness skin subcutaneous flaps. Their rationale is discussed below.
There are recent reports in the literature that directly and indirectly support the aesthetic benefit of the brow shape and position advocated here and the failure of conventional open and, particularly, closed endoscopic techniques in achieving this look.6,25,26 Freund and Nolan6 had nine cosmetic surgeons and 11 cosmetologists evaluate eyebrow position and shape using computer-graphic manipulation of photographs. They also had these observers compare 100 preoperative and postoperative brow lift photographs taken from 16 frequently referenced articles. They concluded that the medial brow should be at or below the supraorbital rim but not above it, that eyebrow shape should have an apex lateral slant, and that standard open brow lifts frequently result in unsatisfactory eyebrow height and shape as judged by these criteria.

Swift et al.25 evaluated brow position 1 year after endoscopic brow lift in 20 patients. They found that endoscopic brow lift indeed produces a long-term elevation of the brow. However, the elevation medially was consistently greater than that at the level of the lateral limbus and lateral canthus. These authors point out that this type of elevation tended to flatten the brow, which may not be the most aesthetically desirable eyebrow shape and position.

Troilius26 compared long-term brow position after both endoscopic subperiosteal and open coronal subgaleal lifts. He, too, found that the medial brow was raised higher than the lateral brow with the endoscopic lifts and that the average distance between midpupil and brow was 28.9 mm (the normal average distance in a young female adult is 23 mm) (Fig. 1).2 Troilius did not address the aesthetic consequences of these procedures other than to comment in the legend of patients who had open procedures. He said that they looked better postoperatively because their lateral brow was elevated from the preoperative  position.
The aesthetic goal of brow-lift surgery should be restoration of youthful brow shape and position, not elevation perse. As shown in the patient in Figure 11, brow position in youth (Fig. 11, above) is often lower than the posture maintained in later years (Fig. 11, below). Ideal brow positioning, in most cases, requires minimal elevation of the medial brow and significant elevation laterally (Fig. 1).4,6,11 To achieve this, an open coronal approach is used and the corrugator muscles are not excised. The coronal incision allows differential scalp excision and more selective control of brow contour. Brow repositioning alone or in combination with upper blepharoplasty significantly im- proves transverse forehead wrinkles, because patients no longer chronically strain to clear their field of vision.15 The coronal incision and lateral brow lift also allow a more vertical elevation of the lower face, both avoiding the lateral sweep5 and managing the lateral orbital skin excess inherent in vertical midface lifts.9 The corrugator muscles are not excised, because their removal results in elevation and separation of the brow.7,27 Therefore, the brow lift procedure, as described in this study, accepts persistence of dynamic forehead wrinkles in exchange for optimal brow position and contour. As an alternative to corrugator manipulation, significant glabellar frown lines may be treated operatively with dermal fat grafts and postoperatively with botulinum toxin.28,29
The widespread training of craniofacial techniques and, more recently, the use of endoscopic equipment, which allows surgical access through more limited incisions, has resulted in several articles describing cheek elevation as a component in rejuvenation of the lower lid. These methods have evolved from modifications of Tessier’s procedure30 using bicoronal, intraoral, and periorbital incisions,30 –34 to those using small scalp incisions for endoscopic access,35–37 to ones using periorbital incisions alone.38–43 By restoring the cheek-lid interface, these procedures have moved toward restoring a more youthful lid. However, they are often associated with a significant incidence of palpebral fissure distortion that are little documented in the literature44–46 but mentioned in open fora, noted in clinical practice, and perhaps suggested by the multiple generations of these procedures.47 The palpebral fissure tends to vertically elongate with age and may be further compromised by conventional skin muscle flap blepharoplasty.8 Procedures that disassemble and reassemble the lid and lateral canthus, often part of midface lifting procedures, may result in unnatural shapes and positions of the fissure (Fig. 15).

Only recently have Hester et al.9 reported a complication/revision rate of 19 percent related to canthal deformity and lower lid malposition when reviewing their 5-year experience of transblepharoplasty lower lid and midface rejuvenation. This procedure involved skin muscle flap exposure, extensive subperiosteal mid- face and lower lid mobilization, and lateral canthotomy and cantholysis. Hobar and Flood’s48 recent description of a simplified midface lift, similar to the one described here, emphasizes that there is no risk of palpebral fissure distortion with their procedure because no eyelid incision is used.48 Lid and canthal malpositions are not unexpected when aesthetic procedures mimic the complexity of major reconstructive ones.
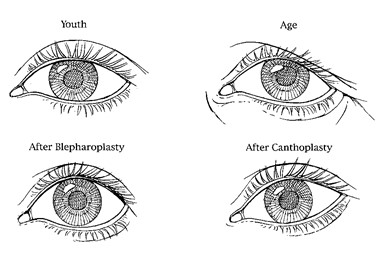
The concepts and surgical techniques for orbital rejuvenation presented in this  study evolved from the author’s training in and experience with orbital reconstruction using craniofacial techniques. Craniofacial approaches for orbital reconstruction use remote incisions to allow complete separation of the soft tissues from the underlying skeleton in the subperiosteal plane. Previous objective evaluation of these soft-tissue approaches for orbital reconstruction revealed the following points germaine to the rejuvenation of the cheek and lower lid.49 Use of the blepharoplasty skin muscle flap to expose the lower lid often distorts the shape of the palpebral fissure by increasing its vertical height. It was found that it was difficult to restore the precise position of the lateral canthus and the shape of the lateral commissure after the canthus was detached and repositioned. The cheek soft tissues were found to sag if they were stripped from the anterior face of the maxilla and not resuspended. This sag results in a loss of cheek prominence, accentuation of the nasolabial fold, and possible vertical elongation of the palpebral fissure—findings not dissimilar from those resulting from the aging process. Resuspension of the cheek soft tissues reversed these distortions.50 This analysis revealed the importance of palpebral fissure shape in the presentation of the upper face. It also emphasized that the predictability of soft-tissue healing and external landmark appearance was related to the extent of soft-tissue manipulation. A clinical approach was, therefore, adapted whereby the risks of extensive soft-tissue degloving were confined to the more devastating posttraumatic orbital deformities.51 This experience in- fluenced concepts for orbital rejuvenation, which emphasizes the sensitivity of the shape of the palpebral fissure to periorbital soft-tissue manipulation. It is noteworthy that Hester et al.9 have modified their transblepharoplasty ap- proach to rejuvenate the orbit and midface to lower the 19 percent incidence of lower lid and canthal malposition. They advocate less dissection of the lower lid and cheek and avoidance of cantholysis and canthoplasty.
The limited periorbital dissection used in the procedure presented here preserves or improves palpebral fissure shape by several potential mechanisms, including preservation of orbicularis oculi innervation, minimization of scarring, division of the lower lid retractors, recruitment of lower lid skin, and avoidance of lateral canthal reconstruction and repositioning. The innervation to the orbicularis oculi muscle to the lower lid—particularly the pretarsal portion, which is believed responsible for maintaining lower lid tone—is not violated. In a cadaver study, Ramirez and Santamarina recently have shown that innervation to the orbicularis oculi comes from the zygomatic branches of the facial nerve, which enter the muscle’s underside vertically from below.52 Skin muscle flap blepharoplasty, skin muscle flap approaches to the midface, and muscle strip procedures tend to denervate this muscle, thereby predisposing to deterioration of lid tone and position. Preservation of the orbital septum eliminates the possibility of shortening of this lamella with scarring. Less surgical disruption of the lower lid lamellae and their attachment to the skeleton results in less potential for distortion from wound contraction. Division of the lower lid retractors during the retroseptal transconjunctival approach for fat removal may allow the lower lid to assume a more elevated position. Maintenance or improvement of lower lid position also results from the cheek elevation intrinsic to this procedure, which recruits vertical height from the outer lid lamellae. Note that palpebral fissure shape is maintained in the young patient in Figure 11 and improved (made narrower) in the patients presented in Figures 12 through 14.Finally, because there is no manipulation of the lateral canthus, palpebral fissure distortions caused by lateral canthus repositioning with canthopexy or canthoplasty are avoided.
Although protective of the shape of the palpebral fissure, this procedure’s less aggressive separation and rearrangement of lid and cheek tissues provides for a relatively less dramatic effect on the cheek-lid interface and on the tear trough deformity. Similarly, improvements in lower lid contour deformities caused by orbicularis oculi muscle redundancy or hypertrophy may be less marked when accomplished by muscle surface imbrication or trimming than by those techniques using muscle  excision.
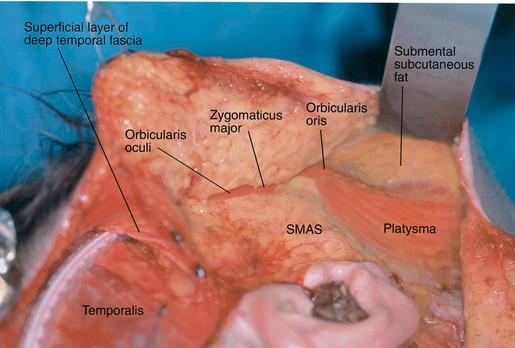
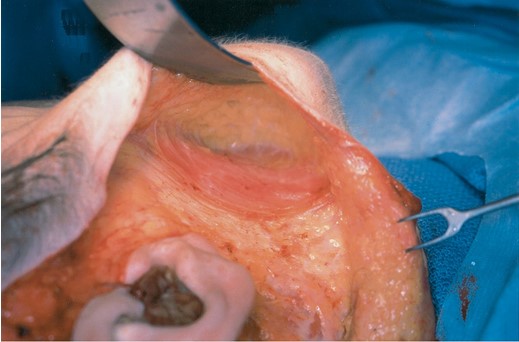
The skin-only face lift described here is different from conventional skin-only lifts53 because all the subcutaneous fat in this procedure is elevated with the flap away from the SMAS and platysma. This plane of dissection, which was advocated by Su and Yaremchuk in 198454 and recently by Hoefflin in 1998,55 has several advantages. Whereas most skin lifts are performed blindly, bluntly, and in a poorly defined anatomic plane, this procedure is done under direct visualization on the well-defined platysma-SMAS-anatomic continuum. All branches of the seventh nerve are located beneath this layer and are, therefore, protected. With the aid of loupe magnification, each vertical perforator leaving the platysma and SMAS can be visualized and coagulated with bipolar electrocautery before being divided. This method is somewhat tedious and time consuming but results in less postoperative bruising. Although the platysma and orbicularis oris may be thin and attenuated in older patients, an extensive medial undermining can be done, allowing safe division of the mandibular retaining ligaments. In addition, having all of the jowl and submandibular fat on the flap allows precise contouring with scissors to optimize mandibular neck contour.56,57 Finally, elevation of a full-thickness skin flap compromises circulation to the skin less than elevation at a more superficial level. Theoretically, this thicker flap allows more extensive undermining and tension at  closure.
SUMMARY
The combining of a subperiosteal brow and midface lift, skin-only lower lid excision, transconjunctival retroseptal fat removal, upper lid blepharoplasty, and full-thickness skin and subcutaneous lower face lift is designed to fulfill the objective criteria of a youthful appearance while minimizing iatrogenic sequelae. This young and “unoperated†look may be summarized as one with brows that have an apex lateral slant, eyes that are narrow, lower lids that are short, cheeks that are full, and a neck that is well defined. The brow and mid- face lift performed through a bicoronal incision allow selective elevation of the lateral brow and a more vertical elevation of the lower face. The midface lift softens the nasolabial fold and restores the cheek prominence and cheek-lid interface. When coupled with a skin-only blepharoplasty and transconjunctival fat removal, lower lid contour is improved without distortion of the palpebral fissure. The full- thickness skin subcutaneous lower face lift allows dissection along the well-defined SMAS platysma anatomic continuum. This plane of dissection is safe to the seventh nerve, allows more precise hemostasis of the vertical perforators, provides a flap with a richer vascularity, and allows precise submandibular fat contouring. This surgery requires that the plastic surgeon be familiar with the periorbital soft tissue, the facial skeletal structure, and the SMAS- platysma anatomy.



Leave Comments
You must be logged in to post a comment.