Improving Aesthetic Outcomes after Alloplastic Chin Augmentation
A novel approach to increase chin projection with alloplastic material is presented. Key aspects of the technique include the consideration of anthropometric normal values in preoperative assessment and planning, a submental approach with wide subperiosteal exposure of the area to be augmented, the use of two-piece porous polyethylene implants for augmentation, and screw fixation of the implant to the mandible. Screw fixation improves the predictability and precision of reconstruction by preventing implant displacement, by obliterating gaps between the implant and the facial skeleton, and by facilitating final implant contouring. In a series of 46 patients (24 primary and 22 secondary) operated on over a 6-year period, this approach allowed anatomically correct, stable chin contours to be created. Iatrogenic problems with macrogenia, mentalis dysfunction, and soft-tissue distortion resulting from implant migration and capsular contracture have been avoided. There have been no infections. Two patients who had had multiple previous chin operations requested revisional surgery to refine contour. {Plast. Reconstr. Surg. 112: 1422, 2003.)
Chin augmentation with implants has long been considered a simple operation that yields gratifying results.1-3 Too often, outcomes are less than ideal. The aesthetic result of alloplastic chin augmentation may be compromised by several factors, which include the preoperative analysis, the surgical technique, the implant design, and the host response to the implant material. For example, the surgeon’s preoperative analysis may deem sagittal chin projection inadequate by subjective criteria that do not take into account sex, the effect of occlusion on lower lip position, the thickness of the chin pad, and the depth of the labiomental fold.3 If these variables are not considered, implant augmentation may result in a chin that is unnatural and too large, particularly in a woman.3
The technique of intraoral placement of chin implants avoids a cutaneous scar hut provides limited exposure to the menton without compromising the mentalis muscle. As a result, the intraoral approach is associated with superior malposition of implants’ and lower lip dysfunction resulting from mentalis muscle division or detachment.3-‘ Alloplastic augmentation with certain shaped implants can create unnatural chin contours. Implants that augment only the chin point produce an abrupt, protruding chin rather than a jaw-chin continuum.5,6 Finally, the host foreign body response to a chin implant may also compromise the aesthetic result. Placement of smooth implants results in the formation of a well-defined fibrous capsule. This encapsulation may result in soft-tissue distortion and implant migration,5-10 causing irregularities and asymmetries.
This article builds on concepts and techniques previously presented by Flowers,5 Terino,6 Zide et al.,3,4,8,11 and Guyuron et al.iu15 to further improve aesthetic outcomes after alloplastic chin augmentation. It adds the use of anthropometric data for both men and women to available preoperative profile assessments. It advocates the use of two-piece, custom-carved, rigidly fixed, porous implants. Their two-piece design allows better conformation of the implant to the contour of the native mandible. Screw fixation of the implant prevents its movement and allows precise “in- place†contouring to ensure the desired augmentation and imperceptible skeleton-implant transitions.1617 Surface characteristics of these implants limit capsule formation and the potential for soft-tissue distortion. This approach has evolved over a 6-year period and has provided successful treatment for 46 patients requesting both primary and revisional surgery.
PATIENTS AND METHODS
Preoperative Assessment
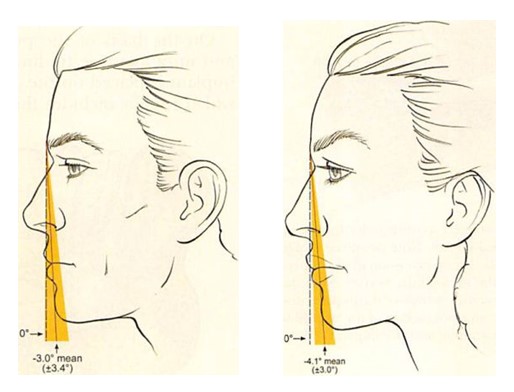
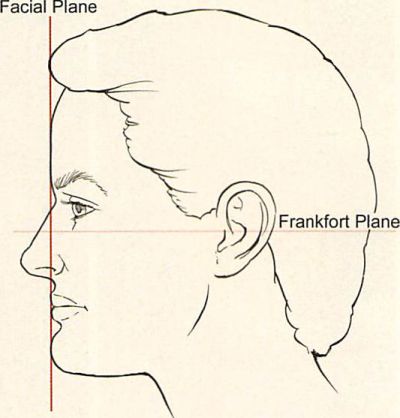
Effective preoperative assessment requires understanding the patient’s aesthetic goals, knowledge of previous facial surgery or orthodontic treatment, and facial examination. Routine radiographic analysis is reserved for secondary surgery. Aesthetic ideals of chin projection should be put in the context both of normative values and of their impact on adjacent soft-tissue landmarks. The anthropometric studies of Farkas et al.IH showed that the mean inclination of the facial profile as defined by a line from the glabella to the pogonion was —3 ± 3.4 degrees in men and —4.1 ± 3.0 degrees in women (Fig. 1). Suggested ideal relationships between the chin and the lips based on normative cephalometric data by different authors19-23 are in consensus that the chin should rest slightly posterior to the lower lip and the lower lip posterior to the upper lip.
Increasing sagittal projection of the chin beyond these relations may risk masculinization of the jaw in women and dysaesthetic deepening of the labiomental fold in some.
Surgical Access
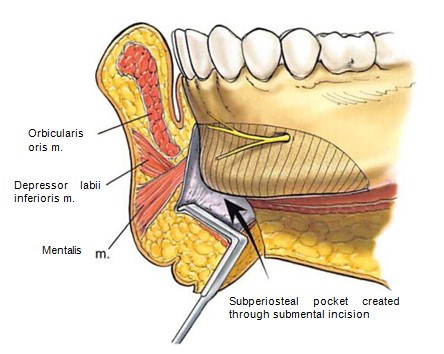
The chin and lower anterior mandible are accessed through a submental skin and subcutaneous incision. Soft tissues are then telescoped over the inferior border of the mandible, where the periosteum is incised with needle tip electrocautery. The midline of the chin is marked on the pogonion as a reference point. Wide subperiosteal dissection is performed. The upper limit of the dissection is the origin of the mentalis muscle. Laterally, the mental foramen with its exiting nerve and inferior border of the mandibular body are exposed. Lateral dissection extends approximately 1 cm beyond the area of augmentation. The submental approach and extended dissection avoid damage to the mentalis muscle, allow visualization of the mental nerve, and provide a perspective of the area to be augmented (Fig. 2).
Figure 1. The inclination of the facial profile as defined by a line from the glabella to the pogonion. The broken line is drawn perpendicular to the Frankfort horizontal at an inclination of 0 degrees. The solid red line represents the mean inclination of the study group. The shaded area encompasses 1 SD. (Isft) The mean inclination in 100 young North American white men was —3 ± 3.4 degrees. (Right) The mean inclination in 100 young North American white women was -4.1 ± 3 degrees (after Farkas, L. G., Hreczko, T. A., and Katie, M. J. Craniofacial norms in North American Caucasians from birth (one year) to adulthood. In L. G. Farkas (Ed.), Anthropometry of the Head and Face, 2nd Ed. New York: Raven Press, 1994. Appendix A.). In both men and women, note that the chin rests slightly posterior to the lower lip and the lower lip lies slightly posterior to the upper lip.
Figure 2. Illustration shows surgical access to the chin and anterior mandibular border. A submental skin and subcutaneous incision is telescoped over the chin where the periosteum is incised with the electrocautery. The striped area denotes die area of subperiosteal dissection. Note that a pocket larger than the implant is dissected to allow ease of implant insertion and to provide a panoramic view of the area to be augmented.
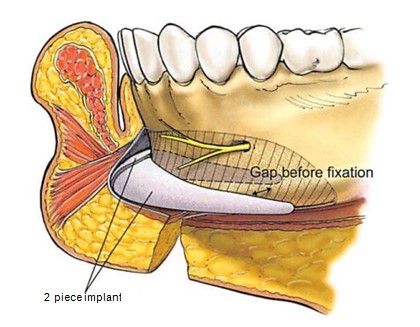
Figure 3. Illustration of a two-piece porous polyethylene implant placed in a subperiosteal pocket. Note two-piece design. The two-piece design allows the lateral extension of the implant to follow the inclination of the mandibular border. Note that because die contour of the posterior surface of the implant does not mimic the contour of the anterior surface of the mandible, there is a gap between the mandible and the implant.
The Implant
The goal of surgery is to create an anatomically correct, stable, mandibular contour. The design and composition of the implant help to accomplish this. Through trial and error with custom-carved chin implants, an easily adaptable implant design has evolved. Its shape and dimensions roughly resemble that of the popular “extended” silicone chin implant design. Il differs in two important aspects.
The chin implant comes in two pieces: a right half and a left half. Segmentation facilitates placement of the relatively long and stiff implant. The two-piece design also provides flexibility in positioning the lateral extensions of the implants, ensuring that it mimics the inclination of the patient’s mandibular body. The lateral extensions differ from “extended implants†in that they have a greater vertical height and more gradual taper. This shape provides a better transition between the implant and the mandible. These features allow the implant to be placed along the mandibular border, thereby creating a new “anatomically correct†shape (Fig. 3).
The implant is made of porous polyethylene (Porex Surgical, Newnan, Ga.). The material’s pore size (100 to 250 /mm in diameter) is such that it allows soft-tissue ingrowth, thereby avoiding clinically apparent capsule formation.24,23 It is firm but flexible and it can be contoured. It is easily fixed with screws. These attributes allow the implant’s inner surface to be adapted to the outer surface of the mandible and for the implant’s outer surface to be shaped precisely, once in place.
Implant Stabilization and Contouring
On the basis of the preoperative assessment and intraoperative findings, an appropriate size implant is placed on the area to be augmented, which usually includes the pogonion, gnathion, and menton centrally and the mandibular border laterally.
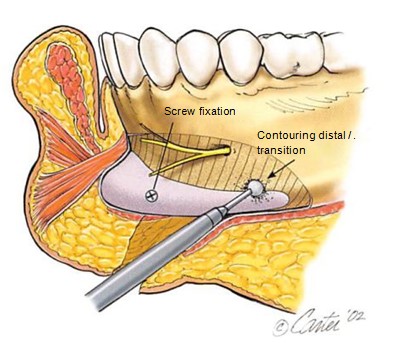
Figure 4. Illustration showing “in-place†contouring of the implant fixed to the mandible with titanium screws. Screw fixation of the implant to the mandible prevents implant movement and obliterates gaps between the implant and anterior surface of the mandible. Screw fixation also allows in-place contouring of the implant to ensure desired contour and an imperceptible implant-skeleton transition.
One or two titanium screws (Synthes Corporation, Paoli, Pa.), 6 to 8 mm in length, are used to fix the implant to die mandible. Screw fixation is performed for several reasons. It allows precise, stable positioning of the implant. It adapts the posterior surface of the implant to the anterior surface of the mandible, thereby obliterating gaps between the implant and the mandible (gaps between the implant and the mandible will result in an undesirable increase in augmentation in the gap area). Immobilizing the implant with screws also allows final in-place contouring of the implant to ensure proper implant projection and an imperceptible transition between the implant and the mandible1617 (Fig. 4).
The wound is closed in layers. A mildly compressive dressing is removed in 48 to 72 hours.
CLINICAL EXPERIENCE
Over a 6-year period, 46 patients (28 women and 18 men) with an average age of 30 years (range, 18 to 54 years) underwent chin augmentation with porous polyethylene implants. Initially, the use of porous polyethylene was reserved for patients referred for secondary surgery. In the past 3 years, porous polyethylene has been used for primary surgery also.
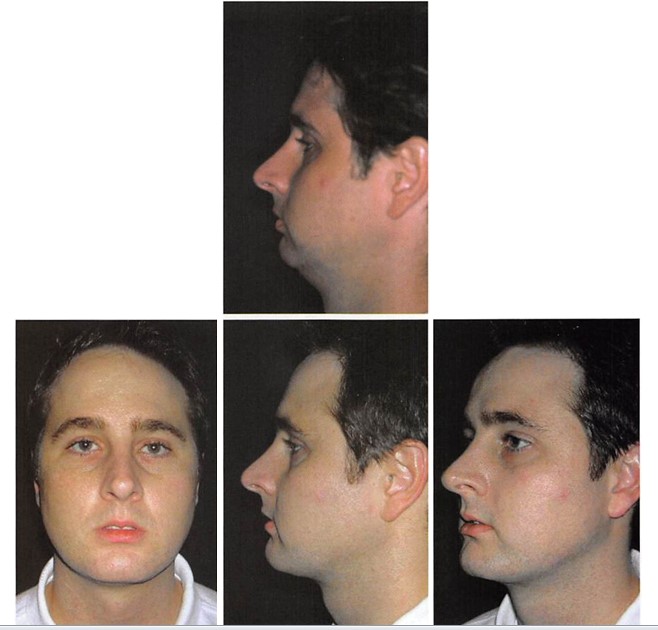
Figure 5. A 31-year-old man underwent chin augmentation with a 7-mm-projection, two-piece, porous, polyethylene implant. A submental lipectomy was performed. (Above) Preoperative frontal and lateral views. (Below) Two-year postoperative frontal, lateral, and oblique views
Twenty-two patients had secondary surgery and 24 underwent primary procedures. Of the 22 patients who had revisional surgery, 21 had silicone implants removed. The remaining patient had a porous polyethylene implant removed and replaced with one of a smaller profile. No patient in this series had an infection. One patient who had had five previous chin augmentation procedures underwent revisional surgery to increase chin projection. A second patient who had had seven previous chin surgeries underwent revisional surgery to correct contour irregularities. Patient examples are shown in Figures 5 through 10.
DISCUSSION
Postsurgical macrogenia, asymmetry, soft- tissue distortions, and lower lip dysfunction in the author’s primary patients and those referred for secondary surgery resulted in a gradual reevaluation of the classic “simple†operation for chin augmentation.1’3,26 Avoidance of these problems required redesigning the operation to the more extensive procedure described here. The goal of this surgery is to create a stable, pleasing chin contour by placing an implant that provides an anatomically correct skeletal shape.
Zide et al.3 have written, and this author agrees, that chin implants may be overused, particularly in women.
Figure 6. A 26-year-old man underwent chin augmentation with a 7-nnn, two-piece, porous, polyethylene implant. (Above) Preoperative frontal and lateral views. (Below) One-year postoperative frontal, lateral, and oblique views.
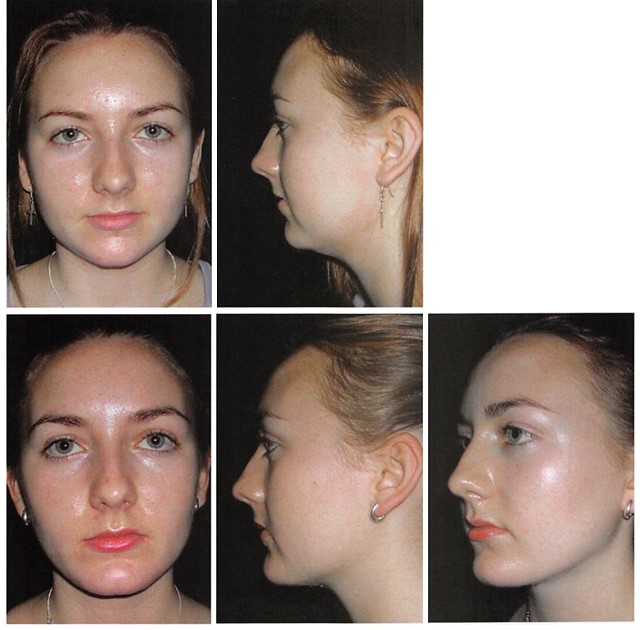
Figure 7. An 18-year-old woman desired more strength and definition to her lower face. A two-piece, o-mm- projection, porous, polyethylene implant was placed. A submental lipectomy and a buccal lipectomy were also performed. The nasal spine was rongeured. (Above) Preoperative frontal and lateral views. (Below) One-year post operative frontal, lateral, and oblique views. Note how augmenting projection 1 SD beyond the “anthropometric female normal†in this patient tends to “masculinize†her appearance on lateral view. Note also how increasing the chin projection almost to that of the lower lip further exaggerates the depth of the labiomental fold.
They offer that this may be so because chin augmentation is deceptively easy to perform and because the surgeon’s evaluation often fails to recognize the possible negative impact of an increased chin projection relative to the position of the lower lip, the labiomental fold, and the thickness of the chin pad.1 Chin implants may also be placed unnecessarily or may be larger than appropriate because widely used subjective criteria allow a greater latitude for augmentation relative to normative values. When McCarthy and Ruff21’ and Farkas et al.27 compared the profile of young North American white adults to classic art and medical illustrations, they found that artists usually portray a larger chin than normally exists in reality. A frequently cited ideal chin projection is adapted from Gonzalez- Ulloa.28,29 His ideal facial plane was a vertical line that extended downward from the nasion to meet the Frankfort horizontal (which extends from the upper margin of the external auditory meatus to the lower orbital ridge).
Figure 8. A 50-year-old woman underwent chin augmentation with a 3-mm, two-piece, porous, polyethylene implant at the time of rhytidectomy. It was placed to lower the most projecting point of the chin. (Above) Preoperative frontal and lateral views. (Below) One-year postoperative frontal, lateral, and oblique views.
This was determined from his analysis of “contemporary beautiful faces and faces known as beautiful through history.â€28 It is redrawn in Figure 11. This ideal is beyond the upper limit of normal for women as determined by the data of Farkas et al.,18 does not take into account sexual dimorphism, and is at variance with ideal lip-chin relations derived from cephalometric studies.18-23 Anthropometric indices are derived from large numbers reflecting a heterogeneous population and cannot be applied to every individual, but average values of the normal face should not be discounted and should be used in the evaluation process. When chin augmentation is suggested as an adjunctive procedure to neck rejuvenation,30-31 the impact of an increased chin projection on overall facial aesthetics should be considered. In their article reviewing results after combining sliding genioplasty with rhytidectomy, Wider et al.32 warned “not to do too much advancing or lengthening,†particularly in women, because some of their patients thought that their new chins were too strong. The combination of chin augmentation and submental recontouring can have a positive effect on facial appearance, provided the increased chin projection is appropriate (Figs. 5, 7, and 8).
The key technical aspects of this more extensive procedure for chin augmentation include the submental approach, wide subperiosteal exposure, and screw fixation of the implant.
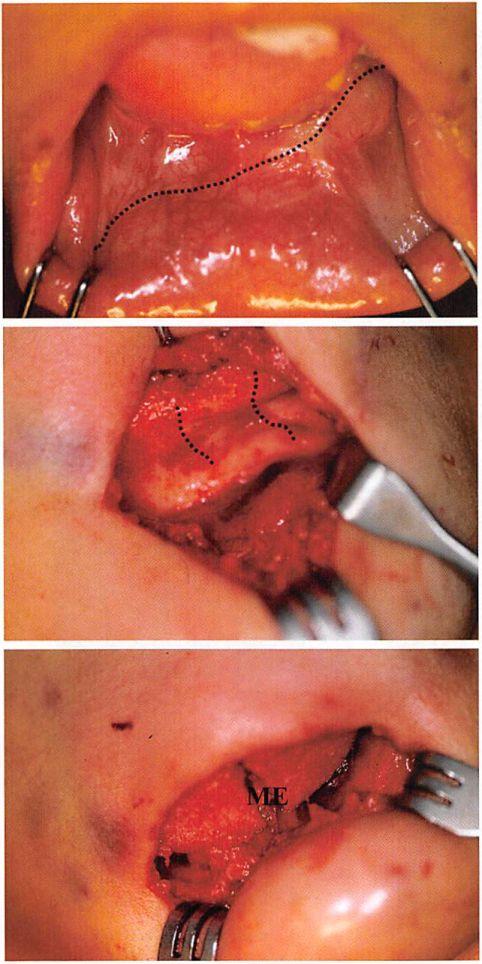
Figure 9. A 36-year-old woman presented 17 years after previous smooth silicone chin implant placement. She was displeased with the asymmetry and the unnatural appearance of her chin. She was concerned that her implant would extrude intraorally. Through a submental approach, the silicone implant was removed. An asymmetric deep bone erosion (approximately 3 mm) was filled with a piece of porous polyethylene, and bone spicules were burred smooth. An extended two-piece, porous, polyethylene implant with 5-mm projection was then positioned, fixed with screws, and contoured appropriately. A submental lipectomy was also performed. (Above) Preoperative frontal and lateral views. Note chin asymmetry, lack of lateral transition, and obliterated sulcus. (Below) Eight-month postoperative frontal, lateral, and oblique views.
At the expense of a well-placed scar, the submental approach avoids injury to the mentalis muscle, a problem often associated with the use of the intraoral approach.311 The submental incision allows excellent access for wide subperiosteal exposure and a panoramic view of the complex and varying contours of the mandible in addition to precise implant placement. Screw fixation of the implant increases the predictability of the operation not only by preventing intraoperative and postoperative movement of the implant but also by eliminating gaps between the implant and mandible.
Figure 10. Intraoral and intraoperative views of patient presented in Figure 9. {Above) Preoperative intraoral view. Broken line follows upper border of asymmetrically positioned implant. Note protruding edge of implant. {Center) Intraoperative view of native chin after implant removal. The black lines follow the surface of the mandible made uneven by erosion beneath the smooth implant. {Below) Intraoperative view of 5-mm-projection, two-piece, porous, polyethylene implant. The eroded area was filled with a piece of porous polyethylene. ME, position of menton.
A gap may occur where the posterior surface of the relatively stiff porous polyethylene implant is not congruent with the anterior surface of the mandible. Gaps between the implant and the mandible equate with unanticipated increases in skeletal augmentation. Stable fixation of the implant also allows, if necessary, in-place contouring of the implant to ensure desired implant shape and imperceptible implant- skeleton transitions.
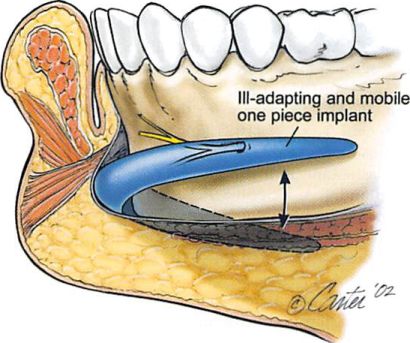
The two-piece design offers advantages over conventional one-piece implants. It facilitates placement of a large implant through a limited access. More importantly, segmentation of the implant increases flexibility in implant positioning. A one-piece implant, particularly one with lateral extensions, is unlikely to have an arc, projection, and inclination appropriate for every mandible. A two-piece design allows adaptation of each of these parameters for a given mandible. When placed through the submental approach, the two-piece implant limits asymmetry in the horizontal plane. With one- piece implants, asymmetry in horizontal positioning increases as one proceeds laterally. It is not uncommon to find one end of an extended silicone implant impinging on the mental nerve, while the other end extends beyond the edge of the mandibular border (Fig. 12).
Figure 11. Gonzalez-Ulloa’s ideal facial plane was a vertical line that extended down from the nasion to meet the Frankfort horizontal. The anteriormost projection of the lips and chin meets this line.
The porous surface of the implant avoids problems related to the capsule formation seen with smooth-surfaced implants. This reactive process predisposes to implant movement, to bone erosion beneath the implant, and to soft- tissue distortion over the implant. The underlying bone resorption has long been recognized33-35 but, in most cases, is thought to have little impact on the long-term result.3’’ However, when implants are placed high on the chin, tooth root erosion may occur, particularly in those with hyperactive mentalis muscles.31’ The bone erosion that occurs beneath smooth implants becomes problematic during secondary chin surgery because of the resultant uneven surface contour (Fig. 10).
Figure 12. Illustration shows that the curvature, posterior surface, and lateral inclination of a one-piece implant may not he appropriate for a given chin and anterior mandibular anatomy. The large subperiosteal pocket required for placement of extended implants may result in postoperative displacement and malposition unless the implant is immobilized. Asymmetry in (he horizontal plane increases with increasing distance from the midline.
The soft- tissue response to smooth implants can be distorting. Large implants placed under thin skin often result in an undesirable outline of the implant9 (Fig. 9). Severe soft-tissue distortion has been reported after removal of silicone implants.37,38 Immediate sliding genioplasty37,38 or replacement with a smaller implant3 has been recommended to limit the contraction process and accompanying soft-tissue distortion. Unlike the experience with smooth- surfaced implants, clinically apparent encapsulation after porous polyethylene implantation has not been seen in a large and lengthy (>13 years) personal series of patients in whom this porous surfaced material was used.25 Available porous polyethylene facial implants have a continuous system of interconnecting pores of approximately 100 to 250 pm in diameter. Animal studies have shown that a pore size greater than 100 pm encourages tissue ingrowth.39’10 Clinical specimens of implanted porous polyethylene have shown a thick connective tissue membrane that was contiguous with the in- grown tissue rather than the dense connective tissue capsule seen with smooth-surfaced implants.21 This fibrous tissue ingrowth allows relative host incorporation as opposed to the host encapsulation seen with smooth-surfaced implants.
ACKNOWLEDGMENT
This study was supported by The Maxwell Blum Scholarship Fund.
REFERENCES
1. Millard, D. R. Adjuncts in augmentation mentoplasty and corrective rhinoplasty. Plast. Reconstr. Surg. 36: 48, 1965.
2. Spear, S. L., and Kassan, M. Genioplasty. Clin. Plast. Surg. 16: 695, 1989.
3. Zide, B. M., Pfeifer, T. M., and Longaker, M. T. Chin surgery: I. Augmentation—The allures and the alerts. Plast. Reconstr. Surg. 104: 1843, 1999.
4. Zide, B. M. The mentalis muscle: An essential component of chin and lower lip position. Plast. Reconstr. Surg. 105: 1213, 2000.
5. Flowers, R. S. Alloplastic augmentation of the anterior mandible. Clin. Plast. Surg. 18: 107, 1991.
6. Terino, E. O. Alloplastic contouring in the malar-midface-middle third facial aesthetic unit. In E. O. Terino and R. S. Flowers (Eds.), The Art of Alloplastic Facial Contouring St. Louis: Mosby, 2000.
7. McCarthy, J. (‘»., Ruff, L. G., and Zide, B. M. A surgical system for die correction of bony chin deformity. Clin. Plast. Surg. 18: 139, 1991.
8. Zide, B. M. Chin disfigurement following removal of alloplastic chin implants (Discussion). Plast. Reconstr. Surg. 88: 68. 1991.
9. Guyuron, B., and Kadi, J. S. Problems following genioplasty. Clin. Plast. Surg. 24: 507, 1997.
10. Ramirez, O. M. High-tech facelift. Aesthetic Plast. Surg. 22: 318, 1998.
11. Zide, B. M., and McCarthy, ). The mentalis muscle: An essential component of chin and lower lip position. Plast. Reconstr. Surg. 83: 413, 1989.
12. Michelow, B. J., and Guyuron, B. The chin: Skeletal and soft-tissue components. Plast. Reconstr. Surg. 95: 473, 1995.
13. Guyuron, B., and Raszewski, R. A critical comparison of osteoplastic and alloplastic augmentation genioplasty. Aesthetic Plast. Surg. 14: 199, 1990.
14. Guyuron, B. Genioplasty. Boston: Little, Brown, 1992.
15. Guyuron, B., and Michelow, B. ). Practical classifications of chin deformities. Aesthetic Plast. Surg. 19: 257. 1995.
16. Yaremchuk, M. J., and Israeli, D. Paranasal implants for correction of midface concavity. Plast. Reconstr. Surg. 102: 1675, 1998.
17. Yaremchuk, M. J. Mandibular augmentation. Plast. Reconstr. Surg. i 06: 697, 2000.
18. Farkas, L.. Hreczko, T. A., and Katie, M.J. Craniofacial norms in North American Caucasians from birth (one year) to adulthood. In I.. G. Farkas (Ed.), Anthropometry of the Head and Face, 2nd Ed. New York: Raven Press, 1994. Appendix A.
19. Steiner, C. C. Cephalometrics in clinical practice. Angio. Orthod. 29: 8, 1959.
20. Hambleton, R. S. Tissue covering of the skeletal face as related to orthodontic problems. Am. J. Orthod. 50: 405, 1964.
21. Burstone, C. J. Lip posture and its significance in treatment planning. Am. J. Orthod. 53: 262, 1967.
22. Ricketts, R. M. Esthetics, environment and the law of lip relation. Am. J. Orthod. 54: 272, 1968.
23. Legan, H. L., and Burstone, C. J. Soft tissue cephalometric analysis for orthognathic surgery. J. Oral Surg. 38: 744, 1980.
24. Wellisz, T., Kanel, G., and Anooshian, R. V. Characteristics of the tissues response to Medpor porous polyethylene implants in the human facial skeleton. /. Long Term Effects Med. Implants 3: 223, 1993.
25. Yaremchuk, M. J. Facial skeletal reconstruction using porous polyethylene implants. Plast. Reconstr. Surg. Ill: 1818, 2003.
26. McCarthy, J. G., and Ruff, G. L. The chin. Clin. Plast. Surg. 15: 125, 1988.
27. Farkas, L. G., Sohm, P., Kolar, J. C., Katie, M. J., and Munro, I. R. Inclinations of the facial profile: Art versus reality. Plast. Reconstr. Surg. 75: 509, 1985.
28. Gonzalez-Ulloa, M. Quantitative principles in cosmetic surgery of the face (profileplasty). Plast. Reconstr. Surg. 29: 186, 1962.
29. Gonzalez-Ulloa, M., and Stevens, E. The role of chin correction in profileplasty. Plast. Reconstr. Surg. 41: 477, 1968.
30. Newman, J., Dolsky, R. L., and Mai, S. T. Submental liposuction extraction with hard chin augmentation. Arch. Otolaryngol. 11: 454, 1984.
31. Courtiss, E. H. Suction lipectomy of the neck. Plast. Reconstr. Surg. 76: 882, 1985.
32. Wider, T. M., Spiro, S. A., and Wolfe, S. A. Simultaneous osseous genioplasty and meloplasty. Plast. Reconstr. Surg. 99: 1273, 1997.
33. Bell, W. H. Correction of the contour-deficient chin. J. Oral Surg. 27: 110, 1969.
34. Robinson, M., and Schuken, R. Bone resorption under plastic chin implants. /. Oral Surg. 27: 116, 1969.
35. Friedland, J. A., Coccaro, P. J., and Converse, J. M. Retrospective cephalometric analysis of mandibular bone absorption under silicone rubber chin implants. Plast. Reconstr. Surg. 57: 144, 1976.
36. Matarasso, A., Elias, A. C., and Elias, R. L. Labial incompetence: A marker for progressive bone resorption in silastic chin augmentation. Plast. Reconstr. Surg. 98: 1007, 1996.
37. Cohen, S. R., Mardach, O. L., and Kawamoto, H. K. Chin disfigurement following removal of alloplastic chin implants. Plast. Reconstr. Surg. 88: 62, 1991.
38. Wolfe, S. A. Chin surgery: I. Augmentation—The allures and the alerts, and Chin Surgery: II. Submental ostectomy and soft-tissue excision (Discussion). Plast. Reconstr. Surg. 104: 1861, 1999.
39. Klawitter, J. J., Bagwell,J. G., Weinstein, A. M., and Sauer,
B. W. An evaluation of bone ingrowth into porous high density polyethylene. J. Biomed. Mater. Res. 10: 311, 1976.
40. Spector, M., Flemming, W. R., and Sauer, B. W. Early tissue infiltrate in porous polyethylene implants into bone: A scanning electron microscope study./. Biomed. Mater. Res. 9: 537, 1975.