Infraorbital Rim Augmentation
In patients with recessive infraorbital rims, alloplastic augmentation of the infraorbital rims makes the eyes appear less prominent and improves appearance. Ten patients (seven women and three men) with an average age of 30 years (range, 23 to 45 years) underwent augmentation of the infraorbital rim with alloplastic implants over a 9-year period. With an average follow-up of 3 years (range, 6 months to 6 years), reconstructions have remained stable and satisfactory, with no incidence of infection, infraorbital nerve damage, or palpebral fissure distortion. One patient underwent additional surgery to correct contour irregularities, and one patient requested implant remoral 1 month after surgery. (Plast. Reconstr. Surg. 107: 1585, 2001.)
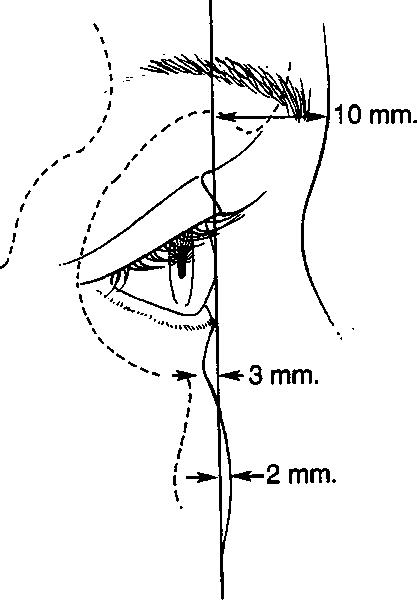
The relationship of the globe to the orbital rims is a primary determinant of the appearance of the upper third of the face. Normal values, that is, averages calculated from groups of young, healthy adults, have been published, and they are presented in Figure l.1″3 On average, the surface of the soft tissues overlying the supraorbital rim lies 10 mm anterior to the cornea, and the surface of the soft tissues overlying the infraorbital rim lies 3 mm behind the anterior surface of the cornea. This implies that the supraorbital rim usually projects 13 mm beyond the infraorbital rim, which is consistent with the anthropometric measurements of Farkas et al.4 When the orbital rims have a greater projection beyond the anterior surface of the cornea, the eyes appear “deep set.†When the orbital rims project less, the eyes appear “prominent.â€
Globe to Orbital Rim Relationships
Fig. 1. Sagittal relations of the anterior surface of the cornea to the soft tissues overlying the supraorbital and infraorbital rims. On average, in the young adult, the supraorbital rim projects 10 mm beyond, the infraorbital rim lies 3 mm behind, and the cheek prominence projects 2 mm beyond the anterior surface of the cornea.1-3
Enophthalmos is the condition in which the globe is positioned too far behind the orbital rims. Most often, this occurs after traumatic disruption of the internal orbit, with a resultant increase in orbital volume and sinkingin of the eye. This problem is corrected by restoring the internal orbital anatomy and, hence, orbital and soft-tissue volume relations to effectively push the globe out. Certain craniosynostoses result in underdevelopment of the frontal bone and midface, with marked projection of the globe beyond the orbital rims. When this disproportion is severe enough to cause symptoms of corneal exposure or to be disfiguring, osteotomies are performed to allow skeletal advancement and improvement of globerim relationships. When globe-rim disproportions are less severe, they are usually left untreated.
Augmentation of the frontal area with alloplastic materials, particularly methylmethacrylate, is often performed to improve surface contours in patients undergoing secondary procedures for various craniosynostoses or post-traumatic deformities.5 The malar component of maxillary hypoplasia is routinely corrected with the placement of alloplastic malar implants by aesthetic surgeons.6 Augmentation of the orbital rims, specifically to improve globe-rim relationships in patients with microform variants of congenital deformities or in “normal†patients with prominent eyes, has received litde attention.
Marchac7 noted that prominent eyes could be camouflaged by augmenting the supraorbital rim. He wrote that methylmethacrylate was the most suitable implant but that the use of alloplastic material always had the risk of late complications. No clinical data were presented in his article. Whitaker et al.2 reported on augmentation of the supraorbital rim with onlay bone grafts and pericranial flaps in nine patients to improve globe-supraorbital rim relationships. Infraorbital rim augmentation to improve sagittal globerim relations has received even less clinical documentation. In 1991, Hinderer8 reported the use of lower orbital rim implants to increase orbital depth in six patients and to correct congenital malformations or post-traumatic deformities in another 15. Hinderer preferred the use of cartilage or bone for rim augmentation, and he presented the correction of both post-traumatic and congenital deformities in his article. Without documenting clinical experience, Agban9 and, more recently, Terino10 reported the efficacy of silicone rubber implants in augmenting the infraorbital rim in patients with maxillary hypoplasia. Flowers,11 who has expertise in both periorbital rejuvenation and skeletal contouring with alloplastic implants, has described augmenting the infraorbital rim when correcting the tear trough deformity in certain patients. He believes that suborbital malar hypoplasia often contributes to or exaggerates this deformity. For that reason, he has designed tear trough implants with various lateral extensions designed to correct specific areas of malar hypoplasia. His “comprehensive†design implant involves the entire malar area, including a majority of the infraorbital rim.
This article presents techniques for and clinical experience with the alloplastic augmentation of the infraorbital rim. By improving the sagittal relations between the globe and infraorbital rim, these techniques were used to improve the appearance of the upper third of the face in nine patients. The results have remained satisfactory, with minimal associated morbidity.
PREOPERATIVE EVALUATION
As depicted in Figure 1, in young, healthy adults, the average projection of the soft tissues overlying the supraorbital rim beyond the surface of the cornea is about 10 mm, and the projection of the cornea beyond the soft tissues overlying the infraorbital rim is 3 mm. These relations are the approximate goals of augmentation of the supraorbital or infraorbital rims. In all patients in this series, the disproportion of sagittal globerim relations was obvious. Documenting the amount of disproportion is useful for preoperative planning and postoperative evaluation, and it can be done with measurements by a Luedde exophthalmometer or with lifesize photographs. A Luedde exophthalmometer placed on the lateral orbital rim and placed perpendicular to the anterior surface of the cornea allows more objective comparison of the anterior projection of the cornea and tissues overlying the infraorbital rim.
Surgical Technique
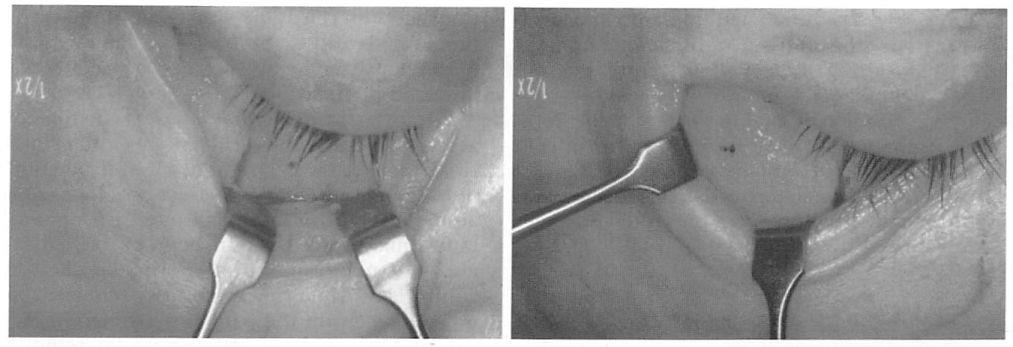
Early in the series, the infraorbital rim was augmented with customcarved pieces of porous polyethylene (Fig. 2). In the last five cases, an implant specifically designed for augmentation of the infraorbital rim was used (Fig. 3; Porex Surgical, Newnan, Ga.). This implant can provide up to 5 mm of anterior projection and is trimmed to meet the specific needs of the patient. A small flange allows it to rest on the most anterior aspect of the orbital floor. This flange allows easier positioning of the implant and a possible area for screw fixation to the skeleton.
Fig. 2. Intraoperative views of infraorbital rim and malar augmentation with custom carved porous polyethylene implants fixed with titanium screws. A transconjunctival incision with lateral canthotomy was used for access. {Left) Infraorbital rim augmentation. {Right) Malar prominence augmentation
The infraorbital rim and adjacent anatomy must be exposed sufficiently to assure ideal implant placement, smooth implant facial skeleton transition, and screw fixation. Direct, subciliary skin or skin-muscle flap incisions can provide this exposure. A transconjunctival incision alone is inadequate for implant placement and screw stabilization. A transconjunctival retroseptal incision, if used, requires lengthening with a lateral canthotomy or combination with intraoral and coronal incisions.
Fig. 3. Implants designed specifically for infraorbital rim augmentation allow up to 5 mm of anterior projection (Porex Surgical). They are carved to meet the specific needs of the patient. Screw fixation assures application of the implant to skeleton, thereby preventing gaps between the implant and the skeleton and aiding a smooth implant-skeleton transition. {Above) Oblique view. {Below) Lateral view.
Fixing the implant to the skeleton with two or three self-drilling titanium screws (Osteomed Corp., Addison, Texas) allows precise application of the implant to the surface of the skeleton. This ensures the desired augmentation, because gaps between the implants and the skeleton effectively result in unplanned increases in augmentation. Screw fixation also allows an imperceptible transition between the area augmented and the adjacent skeleton.
The implants used in this series were not impregnated or irrigated with any antibiotic solution. Intravenous antibiotics (usually a cephalosporin) were administered just before surgery. Oral antibiotics were administered for 5 days after surgery.
CLINICAL EXPERIENCE
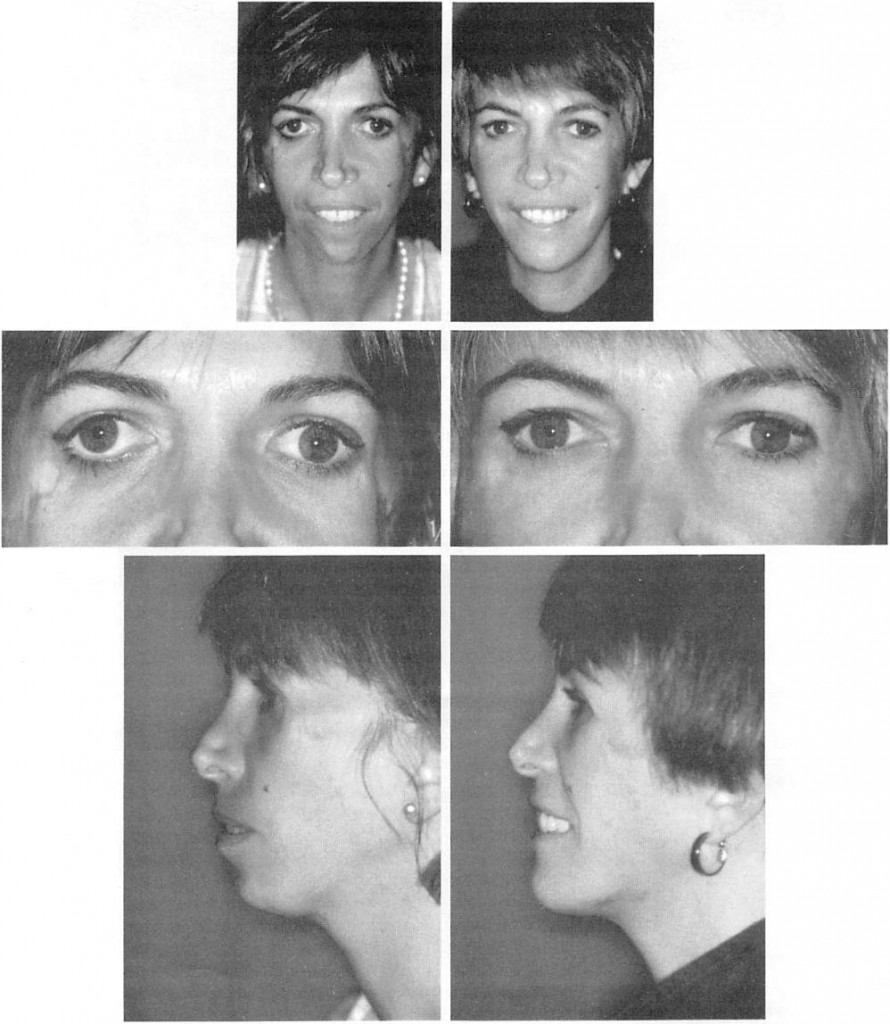
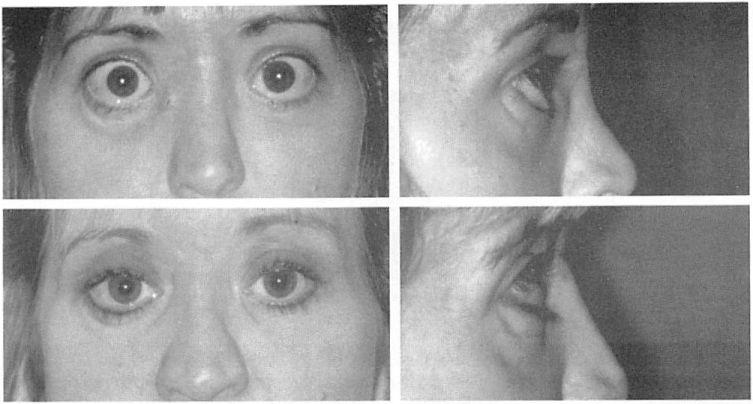
The infraorbital rim was augmented to improve globerim relationships in 10 patients over a 9-year period. The follow-up ranged from 6 months to 6 years, with an average of 36 months. The average age of the three men and seven women was 30 years (range, 23 to 45 years). The cause of the globerim disproportion was maxillary hypoplasia (four patients), Crouzon’s disease (one patient), trauma (two patients), thyroid ophthalmopathy (one patient), radiation-induced growth disturbance (one patient), and Treacher-Collins syndrome (one patient). One of the patients in this series required additional surgery for revision. In one patient who previously had had multiple procedures (Fig. 4), threatened implant exposure was treated with soft-tissue imbrication and implant contouring. One patient requested removal of implants 1 month after surgery because he thought that this surgery made too great a change in his appearance. No infections, palpebral fissure distortions, or symptoms of infraorbital nerve damage occurred. Representative patients are presented in Figures 4 through 7.
DISCUSSION
Globe to orbital rim relations have a wide range of measurements, are influenced by ethnicity and sex, and change with aging. The considerable variability in globe to orbital rim relations is a result of the wide variations in human facial skeleton morphology. Migliori and Gladstone12 determined the normal range of globe protrusion for white and black adults. Using the Hertel exophthalmometer, which measures projection of the anterior surface of the cornea beyond the lateral orbital rim, they found that the range for white adults was 10 mm; for black adults, it was 12 mm. In addition to determining a range of normal values, they documented racial and sexual differences in globe projection. When globe projection was measured relative to the lateral orbital rim, men’s globes, on average, were 2 mm more prominent than women’s, and black men’s and women’s globes were 2 mm more prominent than those of white men and white women.
Recently, Pessa et al.3 discovered that the globe-orbital rim relationship changes with age. They studied two groups of individuals, young and old, using three-dimensional computerized tomography. Their findings are summarized in Figure 8. In the youthful face, the cheek fat lies anterior to the cornea and the orbital fat lies slightly anterior to the orbital rim. The anterior projection of the cheek mass beyond the surface of the cornea has been termed a positive vector.13 With aging, the cheek mass tends to lie posterior to the anterior surface of the cornea (now a negative vector), the orbital fat moves slightly anterior, and the infraorbital rim has a significant movement posteriorly. Hence, retrusion of the infraorbital rim with aging will make the eyes appear more prominent by changing globerim relations, and it will significantly impact the appearance of lower lid bags, particularly in those who tend toward maxillary hypoplasia. Pessa et al.3 hypothesized that it was likely that the infraorbital rim retrusion with aging “unmasked†the fat pads and that infraorbital rim augmentation may become an accepted procedure for lower lid blepharoplasty.
Infraorbital rim augmentation at the time of aesthetic blepharoplasty in patients with orbital rim hypoplasia will have not only a “balancing†but also a “rejuvenating†effect on globe-orbit aesthetics. Furthermore, because rim augmentation makes the relation between orbital fat and the neoorbital rim more like that of youth, less orbital fat removal is required, as was the case with the patient presented in Figure 6. The need for little or no fat removal during aesthetic blepharoplasty when also using extended tear trough implants to augment the infraorbital rim was previously pointed out by Flowers.11 Another “rejuvenating†effect of alloplastic infraorbital rim augmentation can be the improvement of the anterior outline at the interface of the lower eyelid and cheek tissue (Fig. 6). Hamra,14 by modifying Loeb’s technique,13 achieved the youthful “shortlid†> appearance by augmenting the infraorbital rim with intraorbital fat. Hester et al.16 restored the cheeklid interface by combining subperiosteal midface elevation with lower lid blepharoplasty.
The disproportion in globerim relations ‘in all but one of the patients who were operated on in this series was due to maxillary hypoplasia (congenital, iatrogenic, or post-traumatic), and it was clinically obvious in all. Measuring the distance between the anterior surface of the cornea and the infraorbital rim is useful for determining the severity of the deformity and determining the amount of correction necessary to bring patients toward the normal range. Precise, reproducible measurements of the relationship can be done with photoradiography17 and specially designed devices.18,19 These modalities have been used to determine normal values and to plan or evaluate complex periorbital osteotomies performed for craniosynostotic deformities. There are no readily available instruments for accurate, reproducible measurements of this relationship. The Luedde exophthalmometer20 can be used to compare the projection of the globe and the infraorbital rim.
Fig. 4. The first patient treated in this series was a 35-year-old woman with malar and lateral orbital deficiency due to Treacher-Collins syndrome. Silicone implants placed during her teens had been removed because of infection. Rib grafts used to reconstruct the malar and zygomatic area had resorbed, leaving fixation wires visible through thin skin. The zygomatic arch, malar area, and the coloboma of the lateral inf raorbital rim were reconstructed with custom-carved porous polyethylene implants that were fixed with metal screws. Surgery was performed through bicoronal, intraoral, and transconjunctival incisions. In addition, lateral canthopexies and a sliding advancement genioplasty were performed. At 2.5 years postoperatively, an area of implant prominence was treated by imbricating the overlying attenuated soft tissue and contouring the implant prominence. The patient was last seen b years postoperatively and was contacted recently. It has been 9 years since the surgery, and she has had no further surgeries and a stable, satisfactory result. (Left) Preoperative views; (righl) views 2 years postoperatively. (Above) Frontal views; (center) frontal views of orbits; and (below) lateral views.
Fig. 5. A 28-year-old woman with satisfactory occlusion who had suffered panfacial fractures and had undergone multiple reconstructive procedures underwent infraorbital rim augmentation, medial orbital rim osteotomies and repositioning, medial canthopexy, zygomatic arch osteotomy positioning, and lateral canthopexy and resuspension of the midface soft tissues. A cranial bone graft was used to augment the nasal dorsum. Surgery was performed through access provided by bicoronal, intraoral, and transconjunctival incisions. (Above) Preoperative views. (Below) Postoperative view’s at 1 year. (Left) Frontal view’s. (Right) Lateral views.
Fig. 6. A 45-year-old woman underwent augmentation of the supraorbital and infraoi’bital rims, an upper and lower blepharoplasty, and a brow lift. Surgery was done through bicoronal and transconjunctival incisions. At 3 months postoperatively, a poor transition between the implant and frontal bone was contoured under local anesthesia. (Above) Preoperative views. (Below) Postoperative view’s at 6 months. (Left) Frontal views. (Right) Lateral views.
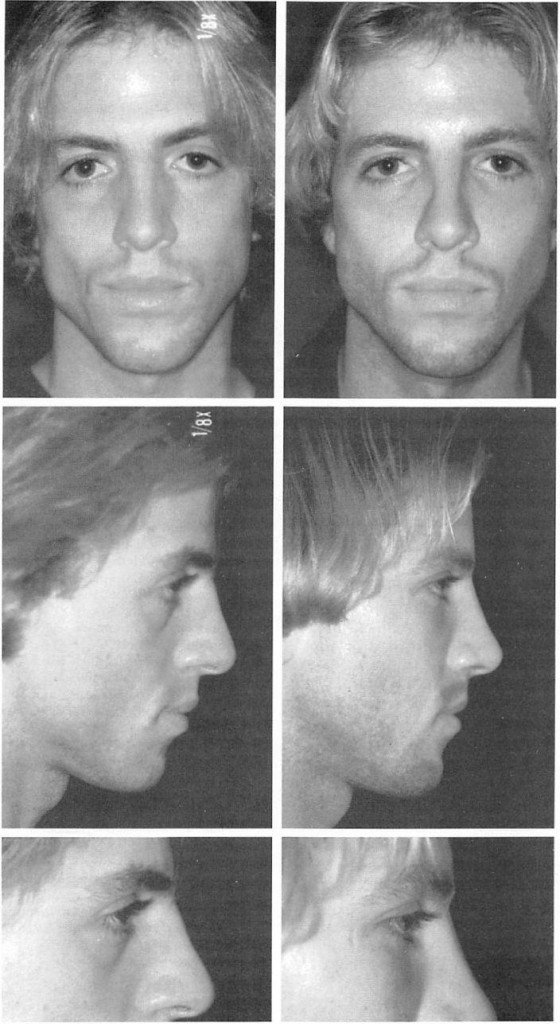
Fig. 7. A 24-year-old man underwent infraorbital rim augmentation, malar augmentation, and rhinoplasty. Surgery was performed through transconjunctival, bicoronal, and intraoral incisions. The infraorbital rim implant depicted in Figure 3 was used. A small style “Morales†implant (Porex Surgical) was used for malar augmentation. (Left) Preoperative views; (right) views 6 months postoperatively.
Fig. 8. Changes in the sagittal position of orbital fat, infraorbital rim, and the cheek prominence that occur with aging.3 (Left) In the youthful face, the cheek mass lies anterior to the surface of the cornea, and the orbital fat lies slighdy anterior to the orbital rim. The position of the cheek prominence beyond the anterior surface of the cornea is termed a positive vector.3,13 (Right) With aging, the cheek mass moves posterior to die surface of the cornea. The infraorbital rim also recedes, and the orbital fat moves slighdy anteriorly. These changes in posiuon of the cheek mass and infraorbital rim were statisdcally significant, but the anterior movement of die orbital fat was not. The position of the cheek prominence behind the anterior surface of the cornea is termed a negative vector.3,13 OF, orbital fat; OR, orbital rim; CM, cheek mass; C, cornea.
This instrument is a handheld transparent ruler that rests on the lateral orbital rim. The position of the cornea and the infraorbital rim are determined by looking through the ruler at right angles to the surface of the cornea. This technique does not control for parallax. Because this measurement is made as part of a preoperative evaluation and is not intended for serial assessment of disease state, the error associated with parallax is accepted.
SUMMARY
The sagittal relationship between the globe and the orbital rims is a primary determinant of the appearance of the upper third of the face. In patients with recessive infraorbital rims due to various causes, alloplastic augmentation of the infraorbital rim can normalize their globe-infraorbital rim relationship and improve their appearance. The results of this procedure are satisfactory, with litde early and no late morbidity.
Michael J. Yaremchuk, M.D.
Division of Plastic Surgery Massachusetts General Hospital, WACC-453 Boston, Mass. 02114 m.yaremchuk@partners. org
REFERENCES
1. Mulliken, J. B., Goodwin, S. L., Pracharktam, N., and Altobelli, D. E. The concept of the sagittal orbital- globe relationship in craniofacial surgery. Plast. Re- constr. Surg. 97; 700, 1996.
2. Whitaker, L. A., Morales, L., Jr., and Farkas, L. G. Aesthetic surgery of the supraorbital ridge and forehead structures. Plast. Reconstr. Surg. 78: 23, 1986.
3. Pessa, J. E., Desvigne, L. D., Lambros, V. S., Nimerick, J., Sugunan, B., and Zadoo, V. P. Changes in ocular globe-to-orbital rim position with age: Implications for aesthetic blepharoplasty of the lower eyelids. Aesthetic Plast. Surg. 23: 337, 1999.
4. Farkas, L. G., Hreczko, T. A., and Katie, M. J. Craniofacial norms in North American Caucasians from birth (one year) to adulthood: Appendix A. In L. G. Farkas (Ed.), Athropometry of the Head and Face, 2nd Ed. New York: Raven Press, 1994.
5. Ousterhout, D. K, Baker, S., and Zlotolow, I. Methylmethacrylate onlay implants in the treatment of fore-head deformities secondary to craniosynostosis. J. MaxiUofac. Surg. 8: 228, 1980.
6. Whitaker, L. A. Aesthetic augmentation of the malar midface structures. Plast. Reconstr. Surg. 80: 337, 1987.
7. Marchac, D. Relationship of the orbits to the upper eyelids. Clin. Plast. Surg. 8: 717, 1981.
8. Hinderer, U. T. Nasal base, maxillary, and infraorbital implants: alloplastic. Clin. Plast. Surg. 18: 87, 1991. 9. Agban, G. M. Augmentation and corrective malar plasty. Ann. Plast. Surg. 2: 306, 1979.
10. Terino, E. O. Facial contouring with alloplastic implants. Facial Plast. Surg. Clin. North Am. 7: 55, 1999.
11. Flowers, R. S. Tear trough implants for correction of tear trough deformity. Clin. Plast. Surg. 20: 403, 1993.
12. Migliori, M. E., and Gladstone, G. J. Determination of the normal range of exophthalmometric values for black and white adults. Am. /. Ophthalmol. 98: 438, 1984.
13. Jelks, G. W., andjelks, E. B. Preoperative evaluation of the blepharoplasty patient: Bypassing the pitfalls. Clin. Plast. Surg. 20: 213, 1993.
14. Hamra, S. T. Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast. Reconstr. Surg. 96: 354, 1995.
15. Loeb, R. Nasojugal groove leveling with fat tissue. Clin. Plast. Surg. 20: 393, 1993.
16. Hester, T. R., Codner, M. A., and McCord, C. D. Subperiosteal malar cheek lift with lower lid blepharo-plasty. In Eyelid Surgery: Principles and Techniques. New York: Lippincott-Raven, 1995.