Making Concave Faces Convex
Abstract. Inadequate projection of the midface skeleton results in midface concavity. Patients with this skeletal morphology tend to have prominent eyes and noses. Lack of skeletal support for the midface soft tissue envelope predisposes to premature cheek descent, resulting in palpebral fissure distortion and lower lid “bags,†an appearance of early aging. Concave midfaces can be made convex with two basic maneuvers performed through intraoral and periorbital incisions. Midface skeletal projection can be increased by augmenting the facial skeleton with alloplastic implants. Multiple implants are required to replicate the complex curvature of the midface skeleton and to avoid impingement on the infraorbital nerve. Subperiosteal elevation of the midface soft tissues and repositioning provides cheek fullness and narrows the palpebral fissure while masking eyelid “bags.†The resultant midface concavity makes the eyes and nose appear less prominent. This procedure has been a safe and effective treatment for 14 patients treated over a 4-year period.
Key words: Facial implants—Midface augmentation—Mid- face-lift—Porous polyethylene
Concave faces often are considered less attractive than convex faces [5,13,14]. The lesser midface skeletal projection intrinsic to concave faces poorly supports the soft tissues, resulting in premature lower lid and cheek descent as well as visible bags [11,17,18]. These faces are “morphologically prone†to further lower lid descent after blepharoplasty [7,9,12,17]. The concave midface also makes the eyes and nose appear prominent.
Severe midface concavity often is seen with the craniofacial dysostoses of Apert and Crouzon. It not only may result in occlusal disharmony, but also may compromise globe protection and airway adequacy. Patients with this morphology require skeletal osteotomies usually at the LeFort III and sometimes at the LeFort I level to remedy ocular, respiratory, and occlusal dysfunction and to improve facial aesthetics.
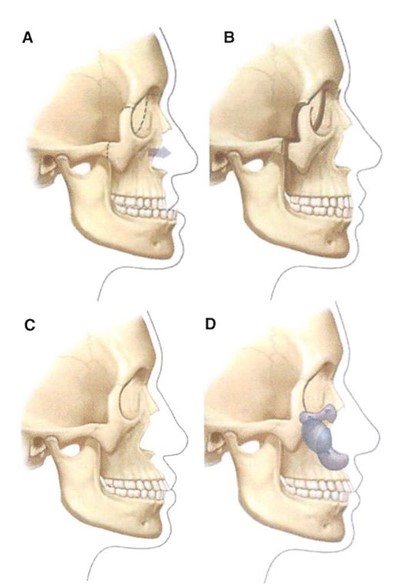
Less severe midface hypoplasia is a common facial skeletal variant [8]. In patients with this morphology occlusion is normal or has been compensated by orthodontics. They have neither respiratory nor ocular compromise. It is in this population that midface skeletal augmentation with multiple implants can simulate the visual effects of skeletal osteotomy and advancement (Fig. 1).
The implants used to effect these changes include those that augment the infraorbital rim [18], the piriform aperture [21], and the malar area [16]. These implants all are modified to meet the specific needs of the patient. Multiple implants are used so that the infraorbital nerve is not compromised, and so that the complex curvature of the skeleton can be mimicked.
This report describes the surgical technique for transforming a concave face to a convex face with multiple implants and a subperiosteal midface soft tissue resuspension. It has been safe and effective for a series of 14 patients over 4 years.
Surgical Technique
Overview
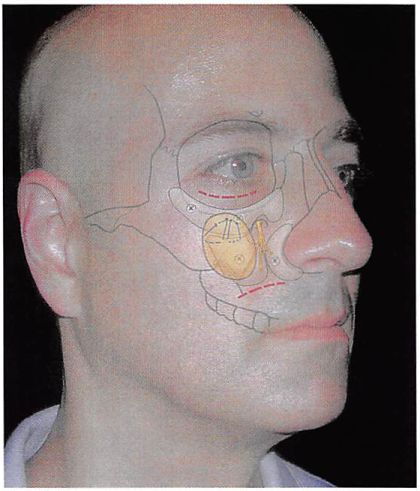
A diagrammatic overview of the operation is presented in Fig. 2. Access to the midface skeleton is obtained through lower lid and intraoral incisions. The entire midface is freed in the subperiosteal plane. The midface skeleton is augmented with a combination of porous polyethylene implants immobilized
Fig. 1. Multiple-implant augmentation of the midface skeleton can simulate the visual appearance of LeFort III osteotomy and advancement without altering dental occlusion. (A) Midface concavity and class 3 malocclusion. (B) Osteotomy and advancement at the LeFort III level provides midface projection and class 1 occlusion. (C) Midface concavity and class 1 occlusion. (D) Multiple midfacc implants provide visual effect of LeFort III osteotomy and advancement, but do not alter occlusion
with screws. The midface soft tissue envelope is elevated and fixed with sutures tied to the infraorbital rim, implant, and/or the lateral orbital rim.
Anesthesia
A general anesthetic administered through nasotracheal intubation is preferred. The nasotracheal intubation protects the airway during the surgery and allows optimal intraoral preparation and surgical access.
Incisions
For accurate positioning of the infraorbital rim implant, a combination of periorbital and intraoral
Fig. 2. Diagrammatic representation of surgical procedures. Broken lines indicate access to midface skeleton. Infraorbital rim, paranasal, and malar implants are applied to the midface skeleton. They are immobilized with titanium screws. The implants are custom contoured to the specific needs of the patient and to provide imperceptible implantnative skeleton and implant-implant transitions. The midface soft tissue envelope, which has been freed by subperiosteal dissection, is elevated and secured by sutures to the rim implant or the orbital rims.
incisions is used. So as not to distort palpebral fissure shape, it is my preference to avoid, if possible, violation of the lateral canthus as well as delamination and relamination of the lower lid.
For that reason, a transconjunctival retroseptal incision alone or in combination with the lateral extent of the lower lid blepharoplasty incision is preferred for access to the upper midfacc skeleton. The entire midface skeleton including the zygomatic arch is separated from its overlying soft tissues by subperiosteal dissection.
The Implant
Usually, three implants are required to increase the projection of the midfacc skeleton, to mimic its contours, and to avoid impingement of the infraorbital nerve. The most important implant is one specifically designed to augment the projection of the infraorbital rim [18]. This implant can provide up to 5 mm of anterior projection. It is trimmed to meet the specific needs of the patient. A small flange allows it to rest on the most anterior aspect of the orbital floor. This flange allows easier positioning of the implant and a possible area for screw fixation to the skeleton. A paranasal implant [21] has been designed to augment the piriform aperture. Usually, implants are carved
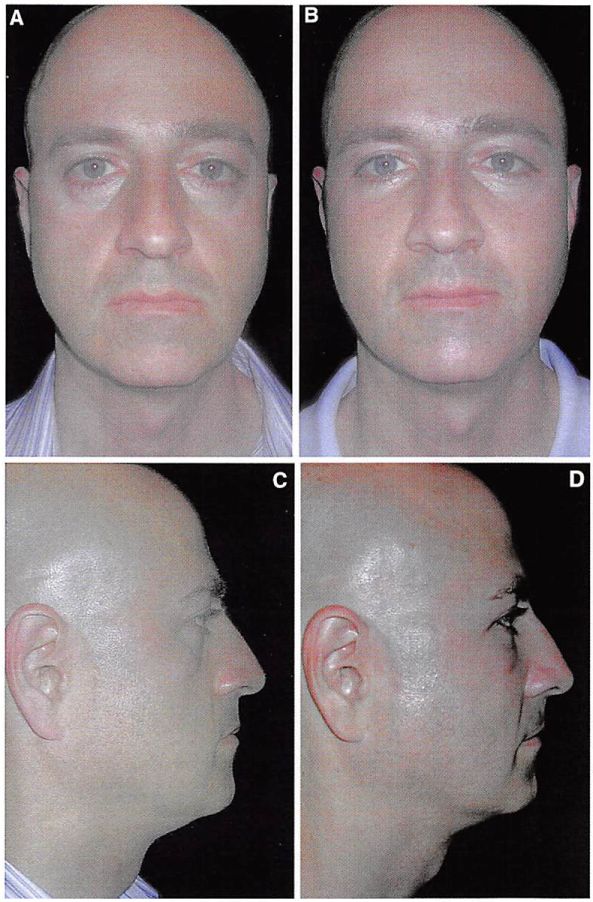
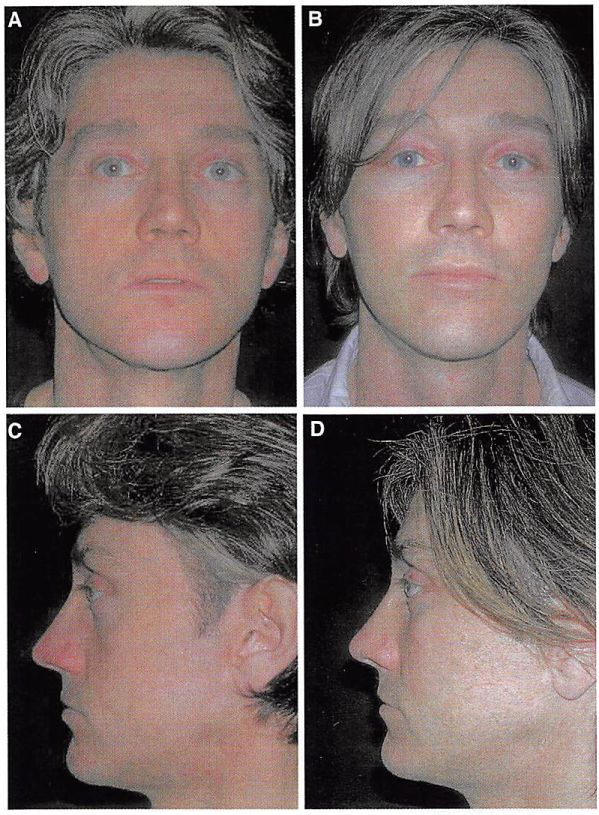
Fig. 3. Preoperative (A.C) and postoperative (C,D) views of a 42-year-old man after multiple
implant midface augmentation and subperiosteal midface elevation.
from a malar design to augment the area below the lateral aspect of the rim implant and the area lateral to the paranasal implant. All implants are immobilized with titanium screws. The implants are trimmed so that there are imperceptible transitions between the implants and the native skeleton.
Soft Tissue Elevation
Through the intraoral incision, a figure of eight suture purchases the cheek soft tissues approximately 3 cm beneath the pupil while a second suture purchases the soft tissues approximately 3 cm beneath the lateral canthus. The sutures are used to elevate the midface soft tissues. They are tied to the infraorbital rim implant or fastened to a drill hole in the lateral orbital rim [17].
A suction drain is placed between the implants and the overlying soft tissues. It usually exits from the temporal scalp. The transconjunctival incision is approximated but not sutured. The intraoral incision is closed in two layers. A temporary tarsorrhaphy suture often is placed to minimize chemosis. The patient is administered intravenous antibiotics intraoperatively and an oral antibiotics for 5 days postoperativcly.
Clinical Experience
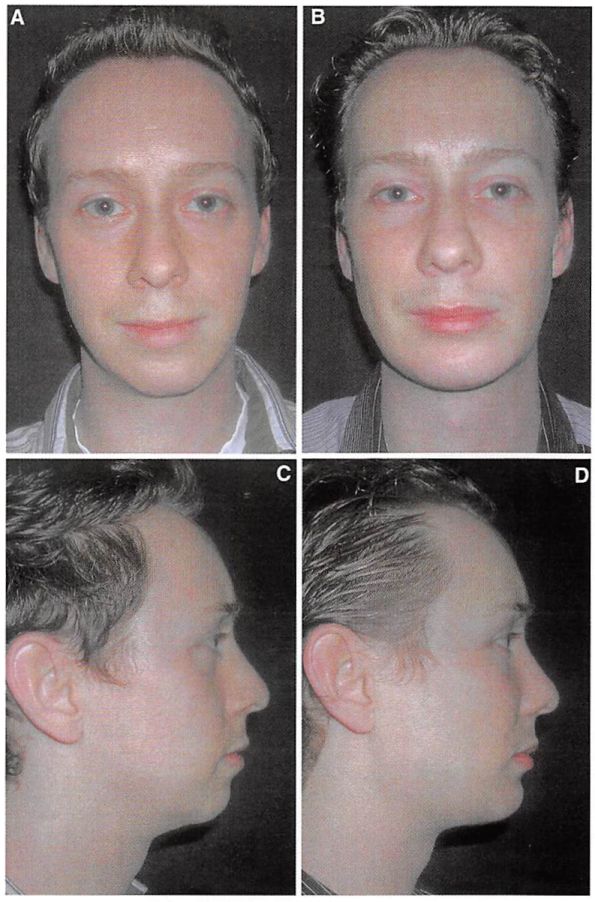
This procedure has effectively transformed concave faces to convex faces for 14 patients (8 men and 6 women) over a 4-year period. Their average age was 41 years (range, 27-56 years). There have been no infections. Two patients required revision of implant shape to improve symmetry. Most patients have altered sensation in the infraorbital distribution for 2 to 12 weeks after surgery. Patients who have undergone this surgery are shown in Figs. 3 to 6.
Fig. 4. Preoperative and postoperative views of a 47-year-old man who had placement of multiple midface implants and midface elevation. Rhytidectomy, upper and lower lid blepharoplasty, and a brow lift had been performed by other surgeons in the past.
Discussion
Patients with midface concavity have an underlying deficiency in maxillary and zygomatic skeletal projection. Ptosis of the cheek and lower lid is accelerated by the lack of skeletal support in this patient population. Facial skeletal augmentation with multiple-screw-fixed alloplastic implants, together with subperiosteal midface soft tissue elevation, can normalize and enhance the appearance of these patients. The technique described in this report is effective and avoids problems inherent to other methods used to produce midface convexity.
If skeletal midface deficiency is accompanied by class 3 malocclusion, LeFort osteotomy (sometimes at two levels) is required to normalize occlusion and to improve globe-rim relations [4,10]. In skeletally deficient patients whose occlusion is normal or has been previously normalized by orthodontics, skeletal repositioning would necessitate additional orthodontic tooth movement. Such a treatment plan is time consuming, costly, and potentially morbid. It is, therefore, appealing to few patients.
The projection of the midface skeleton can be increased by augmenting it with autogenous bone or alloplastic materials. Aesthetic skeletal augmentation is rarely done with autogenous bone because of the unpredictability of the result. Once the graft is revascularized by the host, it becomes subject to osteoclastic activity [2], as determined by mechanical load and soft tissue deforming forces (Wolff’s law). In addition, graft harvest is painful and time consuming. It increases both operating time and recovery time and therefore increases cost. Alloplastic augmentation of the facial skeleton avoids the unpredictability and morbidity inherent in the use of autogenous materials.
I prefer to augment the concave midface skeleton with multiple implants of porous polyethylene fixed with screws. Multiple implants allow precise adaptation to the complex and unique curvatures of each facial skeleton. Furthermore, they allow the operator to avoid implant impingement on the infraorbital nerve that would be inevitable with a single large implant.
Porous polyethylene implants are preferred over smooth surfaced implants for several reasons. The material properties of these implants allow them to be easily carved and immobilized with screws.
Fig. 5. Preoperativc and postoperative views of a 28-year-old man who underwent multiple midface implants and midface elevation. During the same operation, chin and mandible implants were placed, and the vertical height of the chin was reduced.
Their pore size (diameter, 100-250 pm) allows for some soft tissue ingrowth, thereby lessening the fibrotic encapsulation process seen with smooth surfaced implants [15]. Implant encapsulation may result in permanent soft tissue distortion, particularly when large implants are placed under thin skin.
The implants are fixed with screws for the following reasons. Screw fixation immobilizes the implants. This eliminates any intra or postoperative implant movement and subsequent undesirable contour. Their rigid immobilization allows the implants to be contoured “in place†so that there is an imperceptible transition between the implant and the skeleton. Finally, screw fixation allows the posterior surface of the implant to be applied to the anterior surface of the facial skeleton, thereby obliterating any gaps between these two surfaces. Gaps result in an unanticipated increase in projection equivalent to the gap space.
Free fat grafting can be an effective means of augmenting facial contour [1,3,6]. This technique is intuitive for the restoration of soft tissue volume loss attributable to senile atrophy. In my experience, fat injection has a limited role in simulating the effect of an increase in skeletal projection. Whereas augmenting of the facial skeleton results in an increase in the projection of the soft tissue envelope, augmenting of the soft tissue volume results in an inflation of the soft tissue envelope. Overaugmentation of either component brings home the point. If overly large implants were placed on the skeleton, the appearance would be too defined and, ultimately, skeletal. If too much fat were placed in the soft tissue envelope, an increasingly spherical and otherwise undefined shape would result.
Repositioning of midface soft tissues has several benefits. It restores cheek fullness and recreates
Fig. 6. Preoperative and postoperative views of a 50-year-old woman who underwent multiple midface implants and midfacc elevation. In addition, a lateral canthopcxy and mandibular body and angle implants were placed. In the past, the patient had undergone upper and lower lid blcpharoplasty as well as chin augmentation performed by other surgeons.
a cheek-lid interface with a relatively shortened lower lid while narrowing the palpebral fissure shape by raising the lower lid margin [18,19,20],
References
1. Carraway JH, Mellon CG: Syringe aspiration and fat concentration: A simple technique for autologous fat injection. Ann Plast Surg 24:293-296, 1990
2. Chen NT, Glowacki J, Bucky LP. Hong HG, Kim WK, Yaremchuk MJ: The roles of revascularization and resorption on endurance of craniofacial onlay bone grafts in the rabbit. Plast Reconst Surg 1:120-134, 1994
3. Coleman SR: The technique of periorbital lipoinliltra- tion: Operative Techniques. Plast Reconst Surg 1:120- 134, 1994
4. Converse JM, HorowitzSO. Valauri AJ, Montandon D: The treatment of nasomaxillary hypoplasia: A new pyramidal naso-orbital maxillary osteotomy. Plast Reconst Surg 45:527-533, 1970
5. Freihofer HPM: Reversing segmental osteotomies of the upper jaw. Plast Reconst Surg 96:86-91, 1995
6. Guerreosantos J. Haidar F. Paillet JC: Aesthetic facial contour augmentation with microprofiling. Aesth Surg J 23:239-247, 2003
7. Hirmand H, Codncr MA, McCord CD, Hester TR, Nahai F: Prominent eyes: Operative management in lower lid and midfacc rejuvenation: The morphologic classification system. Plast Reconst Surg 11:620-625, 2002
8. Jackson IT, Munro IR, Salyer KE, Whitaker LA: Atlas of craniomaxillofacial surgery Mosby, St. Louis, 1982
9. Jclks GW. Jelks EB: The influence of orbital and eyelid anatomy on the palpebral aperture. Clin Plast Surg 18:193-204. 1991
10. Obwegesser H: Surgical correction of small rctrodis placed maxillae: The dishface deformity. Plast Reconst Surg 45:527-535, 1970
11. Pessa JE, Desvigne LD, Lambros VS, Nimcrick J, Sugunan B. Zadoo VP: Changes in ocular globe-to- orbital rim position with age: Implications for aesthetic blcpharoplasty of the lower eyelids. Aesth Plast Surg 23:337-342, 1999
12. Rees TD, LaTrenta GS.: The role of the Schirmcr’s test and orbital morphology in predicting dry-eye syndrome