Orbital Deformity After Craniofacial Fracture Repair: Avoidance and Treatment
Abstract:
Background and Objectives. To achieve the optimal preoperative appearance following craniofacial fracture repair, the surgeon must be facile in the most sophisticated reconstructive techniques and able to determine their application. The purpose of this article is to describe the common deformities following such repairs, outline a strategy to avoid them, and review the surgical techniques to correct them.
Methods and Materials. The deformities are categorized by the anatomic zones of the orbit, ie, zygomatic, frontal, and nasoethmoidal, affected by low-, middle-, and high-energy impact. The common types of deformity and acute and late treatments are discussed for each category.
Results and/or Conclusions. The optimal time to correct post- traumatic orbital deformities is during the acute phase. Extended open reduction and rigid fixation techniques have their own morbidity, which must not outweigh the deformity of an untreated or partially treated injury. The results of late reconstruction are always limited by scarring of the overlaying soft tissue envelope.
It is difficult to achieve the exact preinjury appearance after the repair of craniofacial fractures. The deviation from normal will depend on the severity of the injury and the techniques available to the surgeon. The energy delivered to the facial skeleton determines the amount of fracture comminution and soft tissue damage. Patients with low-energy injuries have a better chance of being restored to the preinjury appearance than those whose injuries are more severe. High-energy injuries to the orbit require more extensive exposure, fixation, and bone replacement. While extended open reduction and rigid fixation techniques are indispensable in treating high-energy injuries, the unavoidable morbidity associated with these techniques may exceed their benefit when applied to lesser injuries. Therefore, the optimal craniofacial fracture repair requires that the surgeon not only be facile in the most sophisticated reconstructive techniques but also know when to apply them.
Orbital deformities remaining after the repair of traumatic injuries are classified as bone malposition, soft tissue distortion, or globe malposition. In the untreated case, all these deformities arise primarily from the malposition of the bone.
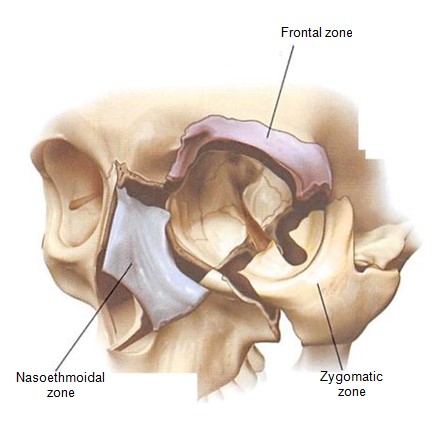 Figure 1. Diagrammatic representation of the orbit divided into three zones — zygomatic, frontal, and nasoethmoidal.
Figure 1. Diagrammatic representation of the orbit divided into three zones — zygomatic, frontal, and nasoethmoidal.
Treatment may not only fail to correct these deformities, but it may introduce new deformities, particularly those of the soft tissues. In this article, deformities in these components are classified by their relationship with the basic anatomic zones of the orbit—zygomatic, frontal, and nasoethmoidal (Figure l). The purpose of this article is to describe the common deformities following trauma repair, the author’s strategy to avoid them, and the techniques to correct them when they do occur.
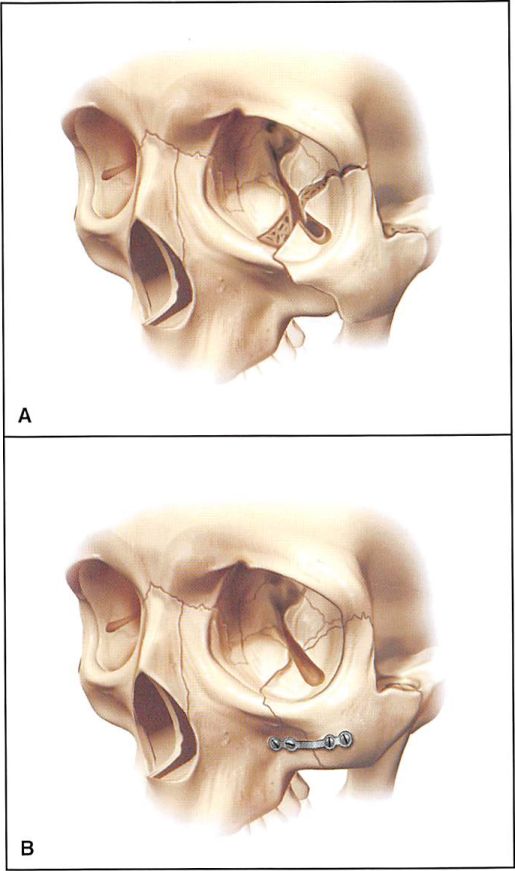
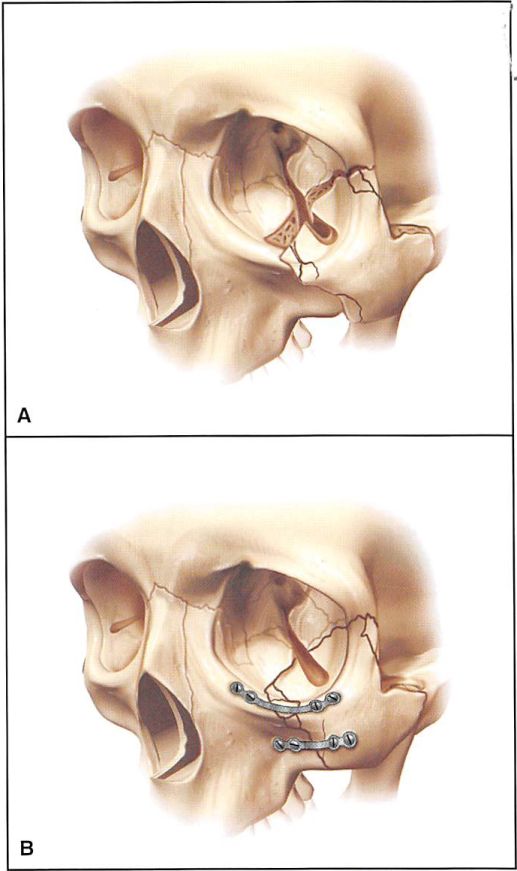
Figure 2. Diagrammatic representation of low-energy zygoma fracture and fixation after reduction. 2A. A low-energy zygoma fracture is hinged at the zygomaticofrontal articulation. 2B. A miniplate at the zygomaticomaxillary buttress is used for fixation.
Figure 3. Diagrammatic representation of a middle-energy zygoma fracture and fixation after reduction. 3A. Middle-energy zygomatic complex fractures are complete at all buttresses. 3B. A miniplate is placed at the buttress, and a microplate is usually placed at the infraorbital rim for fixation.
Figure 4A. Case 1. Preoperative CT scan of a moderate-energy zygoma fracture. 4B. Postoperative appearance 4 months following treatment with the intraoral approach, using reduction and miniplate placement.
ZYGOMA Acute Treatment
Fractures of the zygoma are treated on the basis of segmentation and displacement, which can be determined by axial and coronal computerized tomography (CT) scans.1′ With rare exceptions, all orbital fractures are assessed with axial and coronal CT scans.
Figure 5. Diagrammatic representation of high-energy zygoma fracture and fixation after reduction. 5A. High-energy zygoma fractures are highly comminuted. 5B. Miniplate fixation is required at all buttresses to restore soft tissue deforming forces in these extensive injuries.
These studies not only define the skeletal injury but also provide important data on the status of the soft tissues of the eye and the brain. The data from these two- dimensional (2-D) scans provide a blueprint of the injury, with which the surgeon may plan operative repair. Three- dimensional CT scans, although visually appealing, are similar to an architectural model.
They provide a perspective but less information for actual planning of the reconstruction.’ As defined by Manson et al.1 low-energy injuries, involving the body of the zygoma, are those that are hinged at the zygomaticofrontal suture and have minimal displacement at the infraorbital rim and zygomaticomaxillary buttress. Although some of these injuries may be stably reduced through a Gillies’ approach, the author routinely uses an intraoral approach to reduce the zygomaticomaxillary buttress fracture and stabilizes its position with miniplates. Infraorbital rim position is judged by palpation. This approach avoids any palpebral fissure distortion secondary to surgical exposure of the infraorbital rim (Figures 2A and 2B ).J There are no cutaneous scars. Malar projection is maintained by the plate-and-screw fixation.
Middle-energy zygoma fractures are complete fractures at all buttresses with varying degrees of comminution, usually at the zygomaticomaxillary buttress and infraorbital rim.1 Because of the comminution at the infraorbital rim, open reduction and microplate fixation of the rim is usually required, in addition to open reduction and stabilization of the lateral buttress (Figures 3A and 3B). Infraorbital rim reduction and fixation is performed through a transconjunctival rctroseptal approach. To avoid cutaneous scarring, open reduction or internal fixation are not generally performed at the zygomatico- frontal articulation (Figures 4A and 4B).
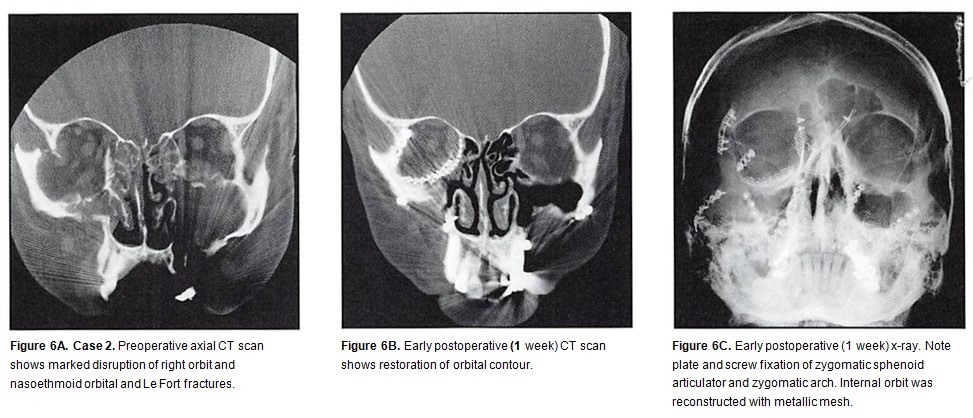
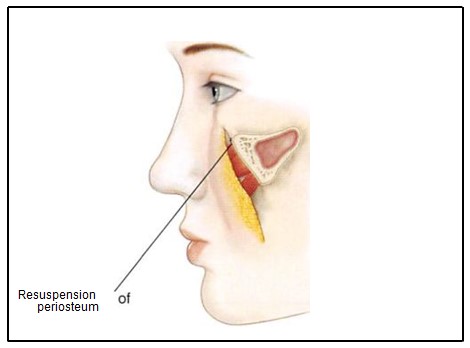
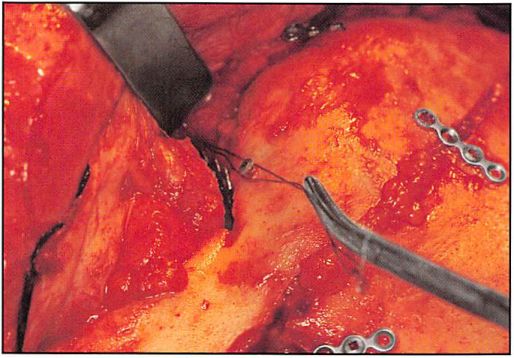
High-energy zygoma fractures usually occur in combination with Le Fort or pan-facial injuries.’ This type of injury exhibits comminution in the lateral orbit and telescoping of the zygomatic arch. These injuries require extended open reduction and rigid internal fixation. Bicoronal, intraoral, and transconjunctival incisions are required, sometimes extended with a lateral canthotomy. The most helpful guide to three- dimensional orientation is restoration of the sphenozygomatic articulation in the lateral orbit. Because there is such a long and complex interface between these bones, two-dimensional reorientation of the bone edges usually implies near-accurate three-dimensional orientation of the entire complex. Anatomic reduction of the zygomatic arch also assures proper projection of the malar prominence. It is important to remember that the zygomatic arch is relatively straight in the anterior/posterior direction, rather than curved.5 To resist the forces that deform soft tissue in these massive injuries, it is usually necessary to provide miniplate fixation at all buttresses (Figures 5A and 5B), although some surgeons consider the micro- or 1.5-mm plates adequate. Because the reduction of multiple fractures requires separation of the soft tissue envelope from the entire skeleton, it is necessary to resuspend the chief soft tissue mass and, if stripped, to replace the lateral canthus (Figures 6A through 6F).6
Common Deformities
Common deformities following zygomatic fracture repair include malar depression, increase in facial width, and descent of the lateral canthal and lower lid.
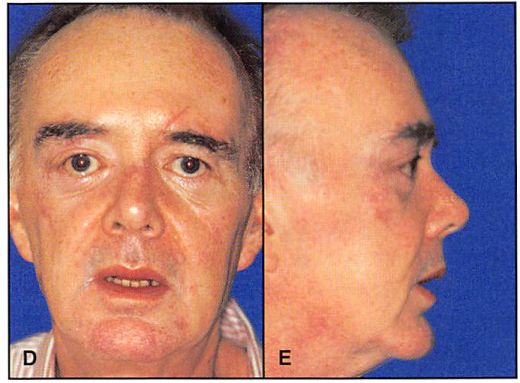
Figure 6D. Postoperative (6 months) clinical frontal view with acceptable restoration of bone architecture. Note that the most noticeable deformity is a slight distortion in the palpebral fissure shape, secondary to exposure for extended open reduction. 6E. Postoperative (6 months) right lateral view.
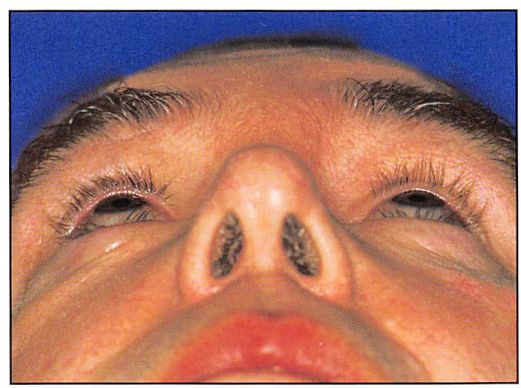
Figure 6F. Postoperative (6 months) “worm’s-eye†view reveals the symmetry of orbital contour and globe position.
Malar depression and an increase in facial width occur when the preinjury position of the malar prominence and the zygomatic arch are not restored or when the position cannot be maintained. Separation of the cheek and orbital soft tissues from the underlying bone — a central component of extended open reduction — may result in lateral canthal, lid. and cheek soft tissue descent, unless these tissues are resuspended to the skeleton at closure. Lid malposition may also result from unfavorable scarring following the use of lower lid exposure techniques.
Late Treatment
When treating zygomatic bone malposition, a decision must be made whether the camouflage techniques or osteotomy and repositioning are necessary.7 After low- or moderate-energy injuries, a lack of malar projection is most often corrected with custom onlay grafting. It is the author’s preference to use porous polyethylene implants, fixed to the underlying skeleton with mini- or microscrews.
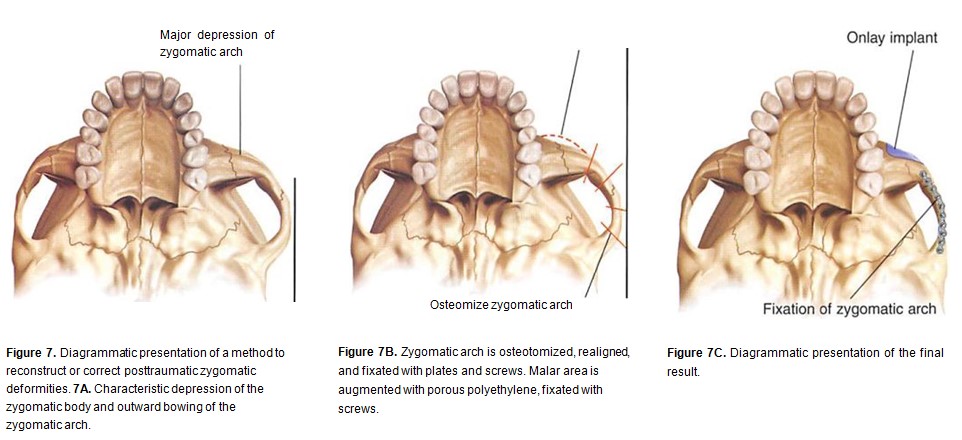
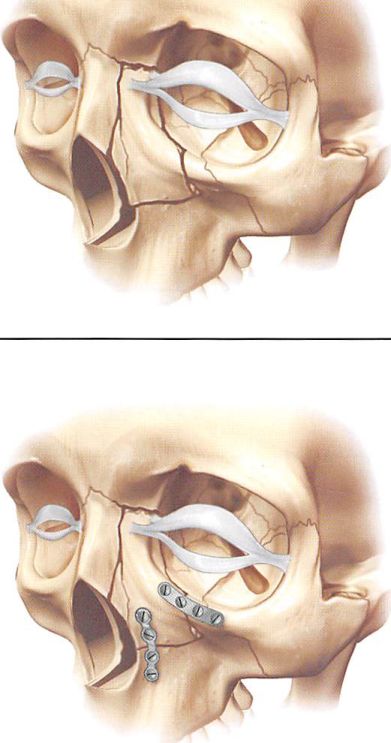
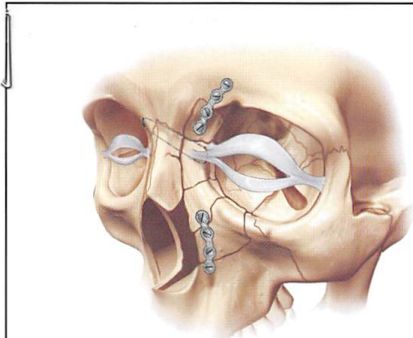
High-energy zygomatic deformities often require extensive osteotomy, repositioning, and cranial bone graft replacement of displaced, partially resorbed, and comminuted bone. A common combination of procedures is osteotomy and repositioning of the zygomatic arch to decrease facial width and custom onlay grafting of the malar prominence (Figures 7A through 7C): it is the author’s preference for use as a basis for onlay grafting. The lateral canthus  and soft tissues of the cheek are repositioned after bone reconstruction is complete (Figures 8A through 9D).
An extensive internal orbital reconstruction is commonly required. An inferior orbitotomy allows an easier and less traumatic retrieval of the orbital soft tissues from the maxillary and ethmoid sinuses. Metallic meshes are indispensable in restoring internal orbit contour and volume.
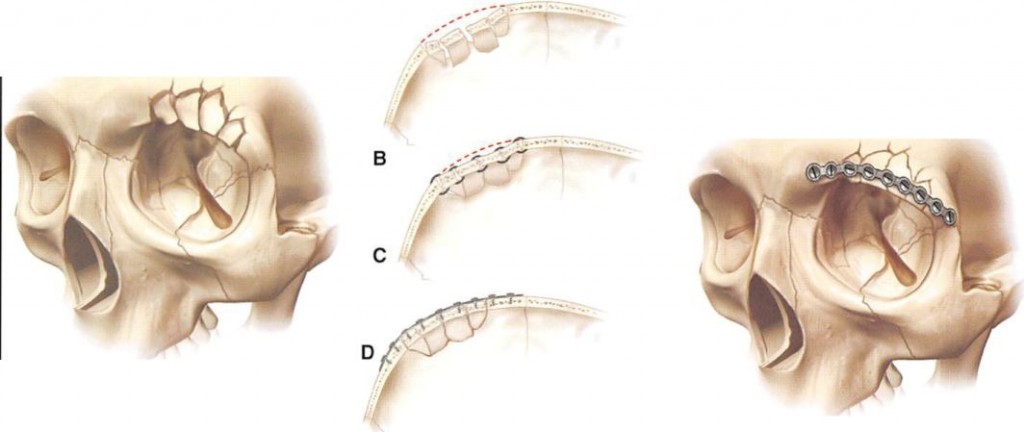
NASOETHMOID FRACTURES
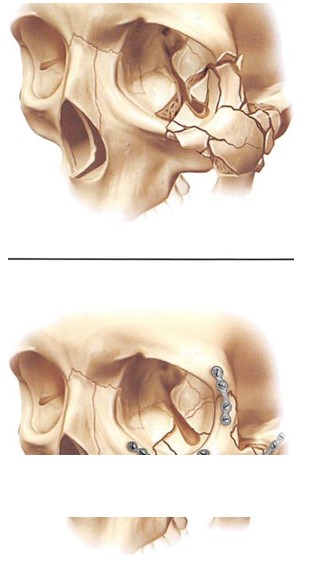
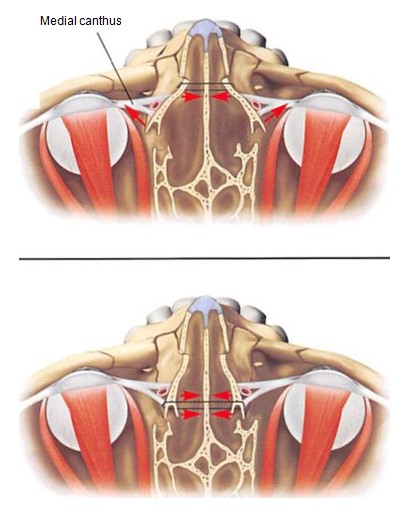
Anatomic replacement of the canthal-bearing bone segment is central to restoring the preinjury appearance of the medial orbital rim in nasoethmoid orbital fractures.8 In low-energy injuries, this canthal-bearing segment is large and may be nondisplaced or displaced only at its inferior articulation. Depending upon the complexity of the adjacent fractures, this segment either is not fixated or is fixated from below at the infraorbital rim and/or central maxillary buttress (Figures 10A and 10B). In higher energy injuries, where comminution is more extensive, the author’s preference is transnasal reduction of the canthal-bearing segment. A wire is placed through drill holes made in the bone behind the canthus, and this transnasal wire is then brought across the nose and stabilized by a miniscrew, placed in the contralateral supratrochlear area (Figure 11). This posterior and superior vector optimizes reduction. When placed anteriorly to the canthus, transnasal fixation will create a vector that splays the canthus outward (Figures 12A through 13H).
If the canthus is detached from the bone segment during the dissection, or if the canthal-bearing bone is too small to purchase with a wire, a transnasal canthopexy is performed. The canthus is identified by incising directly over it. rather than by grasping it from the internal aspect of the coronal incision.
Figure 8. If not resuspended at closure, subperiosteal stripping of the zygoma and malar area results in sagging of facial muscles and subcutaneous tissue, which may lead to changes in palpebral fissure shape with scleral show. 8A. Inferior migration of subcuta¬neous tissue and muscle without resuspension.
Figure 8B. Resuspension of the tissue and suturing to periosteum, infraorbital rim, and temporal fascia.
Figure 10A. Diagrammatic presentation of low-energy nasoethmoid orbital fracture with canthus attached to large bone fragment. 10B. The fracture can be reduced and fixated with plates at infra¬orbital rim and/or central maxillary buttress.
Transnasal canthopexy is never as effective as proper transnasal reduction of the canthal-bearing bone segment with its canthal attachment (Figures 6A through 6F).
Common Deformity
Orbital distortion in nasoethmoid orbital injuries results when the medial canthus is either not repositioned or is repositioned improperly, resulting in telecanthus or vertical malposition of the canthus.
Late Treatment
Telecanthus is best treated during secondary reconstruction by osteotomy of the canthal-bearing bone segment and by repositioning with a transnasal reduction, similar to the technique employed in the acute case.9 If the medial canthus must be moved separately, a separate transnasal canthopexy (in addition to medial orbital rim reconstruction) is performed as described in the foregoing text. It is also important to decrease the interorbital distance by osteotomizing and repositioning the medial orbital rim. Repositioning of the medial orbital rim and the canthus simultaneously avoids the need for any soft tissue rearrangement in the medial canthal area.
SUPRAORBITAL FRONTAL FRACTURES
If the frontal fractures involve the supraorbital rim or roof, they may distort the orbit. Displaced rim fractures require bicoronal exposure and plate-and-screw stabilization to prevent collapse, due to soft-tissue-deforming forces or the compressive forces of interfragment wiring (Figures 14A through 14E).'” When displaced interiorly, roof fractures may cause
Figure 11. Diagrammatic presentation of comminuted nasoethmoid orbital fractures, treated with transnasal wire reduction and fixation.
downward displacement of the globe and proptosis. These injuries always require intracranial exposure to control the brain and allow roof repair or replacement (Figures L5A through 15D).
Common Deformity
Untreated or improperly treated supraorbital fractures usually result in rim and brow depression. If the roof is involved, the globe may be interiorly displaced and proptotic. Loss of the roof and lateral orbit, due to injury and/or debridement with failure to reconstruct the bony anatomy, may result in profound enophthalmos, based on the resultant significant increase in orbital volume.
Late Reconstruction
Severe distortion of the supraorbital rim usually requires osteotomy and repositioning of the rim, often combined with the need for bone replacement, due to bone loss or distortion from comminution and resorption. If the globe is malpositioned due to roof involvement, intracranial/extracranial access is required to protect the brain. Less severe distortions in contour of the rim may be remedied by contouring prominences. Small area depressions are repaired with porous implants, such as hydroxy- apatite cement. Larger areas are usually reconstructed with bone or methylmethacrylate. Most recently, hydroxyapatite cements have been used to restore frontal contour. Porous implants must be anchored with screws to assure their position in the underlying skeleton. Methylmethacrylate is usually fixated by curing or by screws on an anchored grid.
Figure 12. Diagrammatic presentation of transnasal reduction of the medial orbital rims with fixation, placed anterior to the medial canthus, resulting in widening of the nasal base and telecanthus. When placed superior to (12A) and behind (12B) the medial canthus, these transnasal wires maintain medial rim and canthal position.
This fixation limits implant movement and subsequent bone resorption Implant fixation allows the surgeon to contour the implant definitively, with the implant in its final position.
CASE PRESENTATION
Case 1
A 19-year-old patient presented with a moderate-energy zygoma fracture, sustained while playing hockey (Figure 4A). The treatment involved exposure through the intraoral approach, with direct visual access to the zygomaticomaxillary buttress for reduction and palpation of the infraorbital rim. A miniplate was placed at the zygomaticomaxillary buttress. A 4-month postoperative photograph presents the final result (Figure 4B).
Case 2
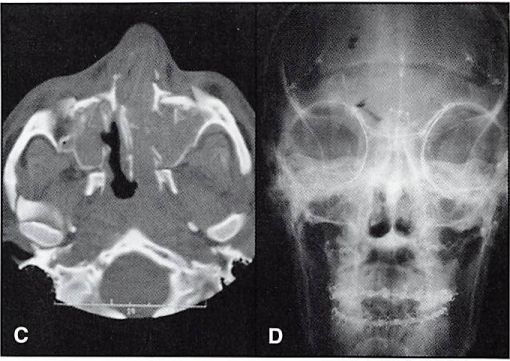
A 52-year-old male patient presented with Le Fort III and nasoethmoid orbital fractures, sustained in an assault. A preoperative axial CT scan showed marked disruption of the right orbit and nasoethmoid orbital and Le Fort fractures (Figure 6A). A postoperative CT scan shows the restoration of orbital contour (Figure 6B). The internal orbit was reconstructed with titanium mesh. A postoperative view was taken with plain film as well (Figure 6C).
Figure 13A. Case 4. Preoperative frontal view of a patient with complex frontal, nasoethmoid orbital, and Le Fort injuries. 13B. Preoperative lateral view.
Figure 13C. Preoperative CT scan shows comminuted central midface with nasoethmoid orbital disruption. 13D. Postoperative (2 weeks) x-ray shows fixation, including transnasal wire and mesh reconstruction of internal orbit.
Figure 13E. Intraoperative coronal view shows transnasal wire fixating right canthal-bearing bone segment.
Figure 13F. Postoperative (18 months) frontal view. 13G. Postopera¬tive (18 months) lateral view.
Figure 13H. Postoperative (18 months) frontal view of orbits
The important guides in anatomic positioning of the right zygoma were alignment and plating at the zygomaticosphenoid articulation, restoration of position. and fixation of the zygomatic arch. The postoperative frontal view (Figure 6D) presents acceptable restoration of bone architecture. Note a discrepancy in the appearance between the reconstructed right medial canthal area and the less injured left side. The bone fragment to which the medial canthus was attached was too small to purchase (obtain) with a transnasal wire. The purchase of the medial canthus with wire and transnasal canthopexy is always less satisfactory than transnasal reduction of the canthal-bearing bone segment. Note from the postoperative right lateral view how failure to resuspend the soft tissue of the cheek results in its descent, with subsequent alteration in palpebral fissure shape and scleral show (Figure 6E). The postoperative “worm’s eye†view shows symmetry of orbital contour and globe position (Figure 6F).
Case 3
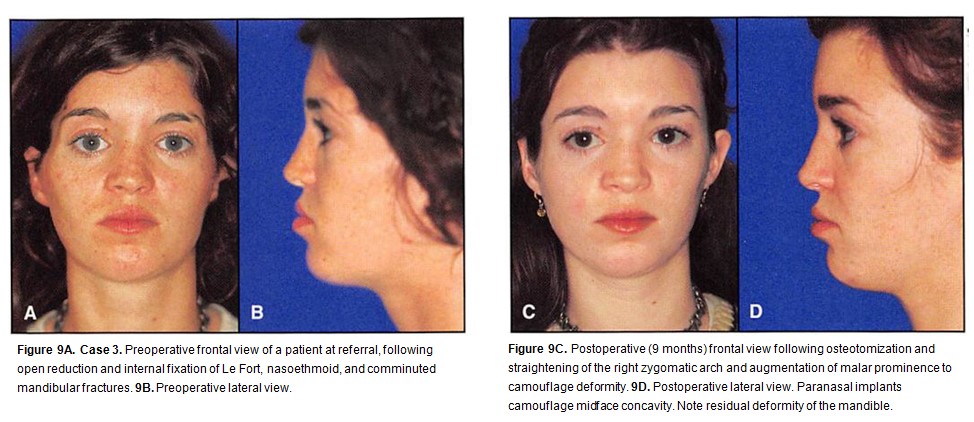
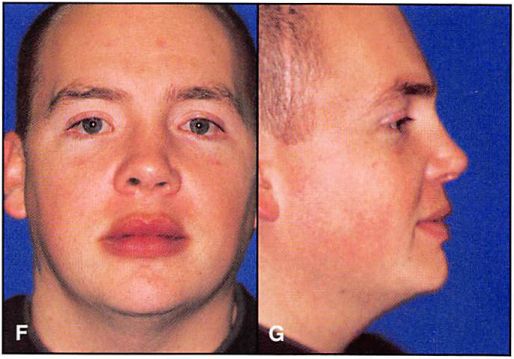
A 24-year-old woman was referred to the author’s institution after an open reduction and internal fixation of Le Fort, nasoethmoid. and comminuted mandibular fractures for the correction of orbital asymmetry and temporal hollowing (Figures 9A and 9B).
Figure 14. Diagrammatic presentation of comminuted injury. 14A. Lateral frontal view. 14B. Axial view showing how comminuted fracture segments tend to collapse, thereby losing projection. 14C. Interfragmentary wire fixation maintains alignment of fracture segments but fails to restore preinjury projection. 14D. Plate-and-screw fixation allows restoration and maintenance of frontal contour. 14E. Frontal view after fixation.
The zygomatic arch was osteotomized and straightened to narrow facial width; methylmethacrylate was used to till out temporal depressions, caused by temporal muscle atrophy. Paranasal areas were augmented with porous polyethylene to camouflage dish face deformity (Figures 9C and 9D).” A residual mandibular asymmetry, however, remained.
Case 4
A 24-year-old male patient presented with frontal and nasoethmoid orbital and Le Fort injuries, sustained in a motor vehicle accident (Figures 13A and 13B). The preoperative CT scan showed comminuted central midface with nasoethmoid orbital disruption (Figure I3C). A transnasal wire was used to fixate the right canthal-bearing bone segment (Figure 13D). The wire was passed across and through the nasal and ethmoid sinuses to be fastened around a miniscrew, placed in the left supratrochlear area. The density beneath the retractor is metallic mesh, used to reconstruct the medial orbit. The post-operative x-ray shows fixation, including transnasal wire and mesh reconstruction of the internal orbit (Figure I3E). Postoperative clinical facial, lateral, and close-up views (Figures 13F through 13H) present the final results.
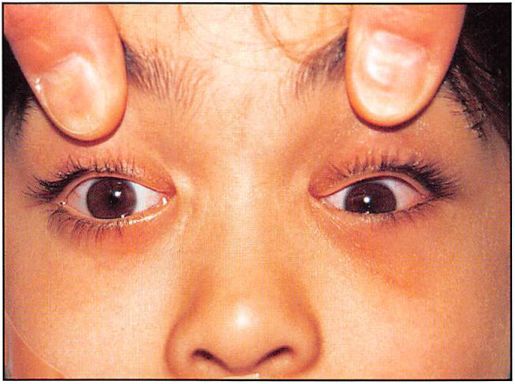
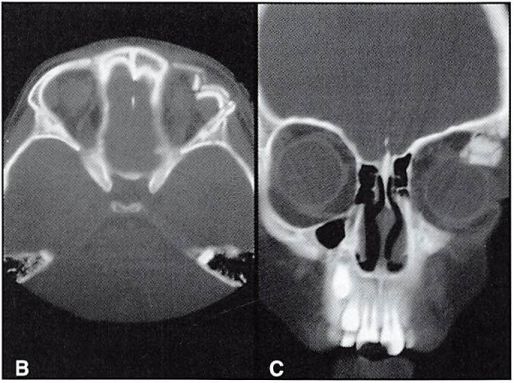
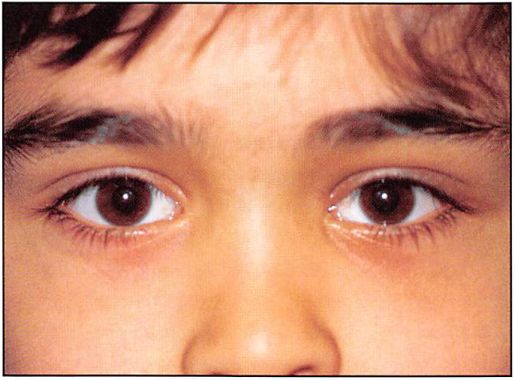
Case 5
An 8-year-old male patient sustained a supraorbital fracture, resulting in proptosis and inferior displacement of the globe (Figures 15A through I5C). A postoperative frontal view of the patient presents the final result, after fixation (Figure 15D).
DISCUSSION
Unlike most fractures of long bones, orbital fractures are not treated to ensure bone healing. The majority of orbital fractures are treated to restore the preinjury skeletal anatomy and, therefore, the preinjury appearance, which is determined by the quality and position of the soft tissue envelope. Extended open reduction and rigid fixation techniques are indispensable in treating high-energy fractures, since the soft tissue deforming forces overwhelm the limited fixation of comminuted fractures, particularly fixation provided by interfragment wiring. The acute phase is the optimal time to correct posttraumatic orbital deformities. Correction at this time allows reapplication of noncontracted flexible soft tissues to an anatomically restored skeletal infrastructure. The algorithm for minimizing orbital deformity in acute-phase orbital fracture repair emphasizes that, although indispensable to the craniofacial surgeon’s armamentarium, extended open reduction and rigid fixation techniques have their own morbidity. This morbidity must not exceed the deformity of the untreated injury or the injury treated by limited means.
Figure 15A. Case 6. Preoperative view of an 8-year-old boy with supraorbital fracture, resulting in proptosis and inferior displacement of globe.
Figure 15B. Preoperative axial CT scan. 15C. Preoperative coronal CT scan.
Figure 15D. Postoperative (6 months) frontal view of the final result
For example, a minor loss of malar prominence or a small step-off at the infraorbital rim is more* acceptable aesthetically than a result where a lower lid incision (used to accomplish a perfect skeletal reduction) leaves the patient with an ectropion or an obvious alteration in the shape of the palpebral Fissure.
With the exception of certain bone contour depressions amenable to onlay grafting, late reconstruction of established orbital deformities usually requires re-creation of the skeletal anatomy through osteotomy and bone and soft tissue replacement and repositioning. Equally important is repositioning the landmarks of the soft tissue envelope. Although the facial skeleton may often be restored to the preinjury configuration, the results of late reconstruction are always limited by scarring contracture and stiffness in the soft tissue envelope.
CONCLUSION
The ideal time to correct posttraumatic orbital deformities is the acute phase. Extended open reduction and rigid fixation techniques have their own morbidity, which must not outweigh the deformity of an untreated or partially treated injury. The results of late reconstruction are always limited by scarring of the overlaying soft tissue envelope.
REFERENCES
1. Manson PN. Markowitz B. Mirvis S. et al. Toward CT-bascd facial fracture treatment. Plast Reconstr Surg 1990;85(2):202-212.
2. Yaremchuk MJ. Del Vecchio DA. Fiala TG. Lee WP. Microfixation of acute orbital fractures. Ann Plast Surg l993;30(5):385-397.
3. Broumand SR. Labs JD. Novelline RA, et al. The role of 3-D CT in the evaluation of acute craniofacial trauma. Ann Plast Surg 1983:31: 488-494.
4. Yaremchuk MJ. Kim WK. Soft-tissue alterations associated with acute, extended open reduction and internal fixation of orbital fractures. J Craniofac Surg 1992:3(3): 134-140.
5. Gruss JS. Van Wyck L. Phillips JH, Antonyshyn O. The importance of the zygomatic arch in complex midfacial fracture repair and correction of posttraumatic orbitozygomatic deformities. Plast Reconstr Surg 1990; 85(6):878-890.
6. Phillips JH. Gruss JS. Wells MD. Chollet A. Periosteal suspension of the lower eyelid and cheek following subciliary exposure of facial fractures. Plast Reconstr Surg 1991:88( 1): 145-148.
7. Yaremchuk MJ. Changing concepts in the management of secondary orbital deformities. Clin Plast Surg 1992; 19( 1): 113-124.
8. Markowitz BL. Manson PN. Sargent L, et al. Management of the medial canthal tendon in nasoethmoid orbital fractures: The importance of the central fragment in classification and treatment. Plast Reconstr Surg 1991:87(5):843-853.
9. Yaremchuk MJ. Revision surgery of nasoethmoid orbital fractures. In: Culbertson JH. Jones G. eds. Operative Techniques in Plastic and Reconstructive Surgery 1998;5(4):334-341.
10. Yaremchuk MJ. Rigid fixation of frontal bone fractures. In: Yaremchuk MJ. Gruss JS. eds. Rigid Fixation of the Craniomaxillofacial Skeleton. Boston. MA: Butterworth-Heinemann; 1992:323-329.
11. Yaremchuk MJ. Israeli D. Paranasal implants for correction of midface concavity. Plast Reconstr Surg 1998; 102(5): 1676-1684.