Restoring Palpebral Fissure Shape after Previous Lower Blepharoplasty
The youthful palpebral fissure can be described as long and narrow. Both the aging process and transcutaneous lower blepharoplasty can cause descent of the lower lid margin and medial migration of the lateral cantlnis, resulting in a rounding of the palpebral fissure. This article presents a technique to correct significant postsurgical lower lid malposition and palpebral fissure distortion without the use of outer or inner lamellar grafts. In overview, subperiosteal dissection frees scarred lid structures and cheek soft tissues, creating a continuous composite Hap. Elevation of the cheek soft tissues recruits deficient outer lamellae and allows the sub— orbicularis oculi fat to be positioned between the orbital rim and scarred lid structures, filling this space and helping to support the repositioned lid margin. Titanium screws placed in the lateral orbit provide a point for secure fixation of elevated cheek tissues. Transosseous wire fixation securely repositions the lateral canthus. This procedure not only restores lower lid position and the vertical height of the palpebral fissure, but it also restores the palpebral fissure’s horizontal length and the lateral canthal angle. It has been effective in correcting palpebral fissure distortion after lower blepharoplasty in 15 patients during a 6-year period. (Plasl. Reconstr. Surg. 111: 441, 2003.)
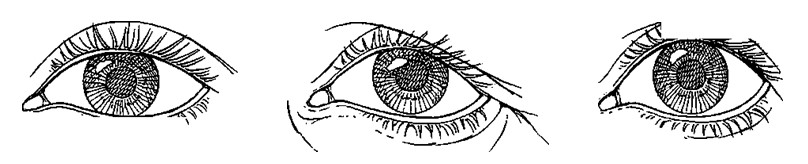
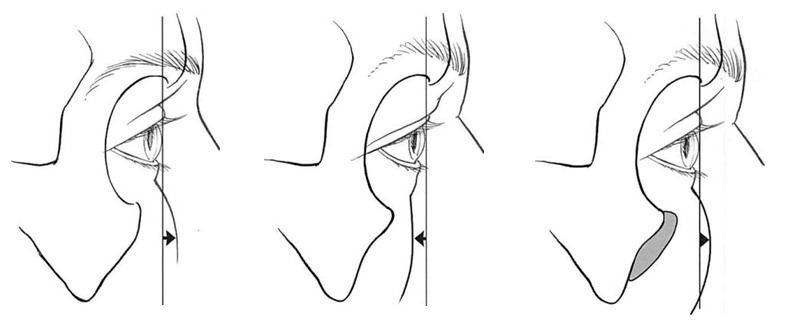
Distortion of the palpebral fissure is a frequent sequela after transcutaneous blepharoplasty. A vertical deficiency of the outer lamellae (skin and muscle) caused by overresection and a shortening of the middle lamella (orbital septum) from scarring causes the lower lid margin to descend and the lateral canthus to migrate medially, resulting in a “round eye.â€1-4 Because the lower lid has been documented to descend and the lateral canthus to migrate medially with aging,1-‘ transcutaneous blepharoplasty often trades an improvement in lid contour for a palpebral fissure more characteristic of the elderly (Fig. 1).
Lower lid descent has long been recognized as the most frequent complication after lower blepharoplasty,8-14 and many procedures have been designed to restore the position of the lower lid relative to the inferior border of the corneal limbus. The lateral canthal malposition and distortion component of the postsurgical round eye, however, has received little attention. Most procedures designed to elevate the lower lid do so by directly shortening the lower lid alone15-17 or in combination with canthotomy, cantholysis, and canthoplasty.18-21 Historically, the lateral can thai/horizontal eyelid shortening procedures were developed as a solution to primarily functional eyelid disorders and were adapted to aesthetic surgery as prophylaxis against or to correct postblepharoplasty lid malposition.22 Nonanatomic reconstructions of the palpebral fissure can be justified when they are necessary to decrease the surface area of exposed cornea and, therefore, ameliorate symptoms of “dry eye.â€23 However, their aesthetic implications should not be dismissed.24
Reviews and extensions of the algorithm of methods to correct lower lid retraction after cosmetic blepharoplasty have been recently published by McCord,25 Fagien,22 and Patipa.2’1 In summary, the algorithm begins with procedures that elevate the eyelid margin by tightening or shortening the lower eyelid horizontally using various types of canthoplasty. More severe deficiencies are treated by adding to the outer lamellae with skin grafts or by recruiting outer lamellae by midface elevation. Finally, it may be necessary to splint the repositioned lid margin with inner lamellar spacer grafts.
Fig. 1. Diagrammatic representation of the palpebral fissure in youth (left), with aging (center), and after blepharoplasty (right). (Redrawn from Yaremchuk, M.J. Subperiosteal and full-thickness skin rhytidectomy. Plast. Reconstr. Surg. 107: 1045, 2001.) The palpebral fissure in youth can be described as one that is long (in horizontal length) and narrow (in vertical height). Aging can cause descent of the lower lid and medial migration of the lateral canthus. After blepharoplasty, overresection of skin and muscle and scarring of the orbital septum can cause descent of the lower lid, with scleral show and medial migration of the lateral canthus, resulting in a “round eye.â€
This article presents an alternative technique for correcting significant postsurgical lower lid malposition and palpebral fissure distortion when lateral canthopexy and lysis of septal scarring alone are inadequate. The technique not only restores the lower lid position and vertical height of the palpebral fissure but also its horizontal length and lateral canthal angle. Moreover, it avoids the use of outer or inner lamellar grafts. Adapted from a long experience with the secondary reconstruction of the posttraumatic orbit,27,28 this technique has effectively restored the palpebral fissure distorted after cosmetic lower lid blepharoplasty in a series of 15 patients during a 6-year period.
SURGICAL TECHNIQUE
Overview
The procedure repositions the lower lid margin and lateral canthus. This is accomplished by first separating scarred periorbital, malar midface, and temporal soft tissues from the underlying skeleton by subperiosteal dissection. In effect, a continuous composite soft- tissue flap is created. Vertical elevation and stable fixation of these tissues allows the lid margin to be elevated, the cheek skin to be recruited to replace deficient outer lamellae, the sub-orbicularis oculi fat to be interposed between the orbital rim and scarred periorbital soft tissues, the lateral canthus to be repositioned, and a smooth transition between the elevated cheek and temporal soft tissues to be created. The technique avoids the use of inter- lamellar dissection and separation and the use of outer or inner lamellar grafts. It is an adaptation of the techniques used to avoid or correct palpebral fissure distortion during complex orbital fracture repair.28,29
Incisions
An intraoral gingival buccal sulcus incision, the lateral extent of a lower lid blepharoplasty incision (without canthotomy), a temporal incision, and the lateral extent of an upper blepharoplasty incision (or a bicoronal incision) are used to access the facial skeleton (Fig. 2).
Soft-Tissue Mobilization
Through the intraoral and the lateral extent of the lower lid blepharoplasty incision, subperiosteal dissection frees the malar midface and scarred periorbital soft tissues (Figs. 2 and 3).
Fig. 2. Surgery is performed through intraoral (broken line), temporal, and lateral extent of the upper and lower lid (without canthotomy) blepharoplasty incisions. A bicoronal approach obviates the need for the upper lid incision. The shaded area represents the area of subperiosteal dissection.
No attempts are made to separate scarred lid lamellae; they are separated from the skeleton en bloc.
Through the temporal and lateral extent of an upper blepharoplasty incision, the temporal and lateral orbital soft tissues are mobilized. In the temporal area, the superficial layer of the deep temporal fascia is incised at the level of the zygomaticofrontal suture to expose the superficial temporal fat pad.30 Dissection is carried along the surface of the superficial temporal fat pad until the zygomatic arch is reached and the subperiosteal plane is reentered.
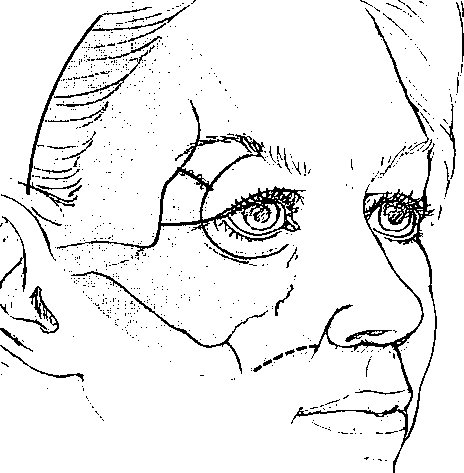
Fig. 3. Sagittal section of lower lid, globe, and orbital rim taken at midpupil. (Above, left) Normal (preoperative relations). (Above, right) After blepharoplasty. Note that aggressive resection of skin and muscle and scarring in the orbital septum pulls the lid margin inferiorly. (Below, left) Subperiosteal en bloc release. Through the lateral extent of the lower blepharoplasty incision, subperiosteal dissection frees the scarred periorbita and cheek soft tissues to create a continuous composite flap. (Belozo, right) Elevated cheek and sub-orbicularis oculi fat. The composite flap has been elevated to reposition the lower lid margin. The cheek skin elevation effectively recruits deficient outer lamellae and also allows the sub-orbicularis oculi fat to be elevated onto the orbital rim to support the repositioned lid margin.
Midface Elevation and Fixation
Through the intraoral incision, 2-0 polyglycolic acid sutures are used to purchase the sub— orbicularis oculi fat and the malar fat pad. The sutures are passed to the lateral lower lid incision, where they are tied to a titanium screw placed in the lateral third of the orbit. After the sutures are tied around the screw, the screw is tightened until the head is flush with the bone surface. The suture in the lateral aspect of the malar fat pad is used as a cable stitch that is tied to the deep temporal fascia at the level of the supraorbital rim. The elevated and stabilized sub-orbicularis oculi fat helps support the freed and repositioned lid margin, and the recruited and elevated cheek tissues replace deficient outer lamellae (Fig. 3, below, right).
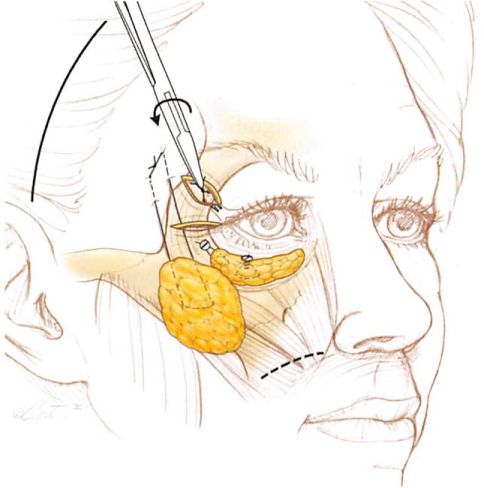
Lateral Canthopexy
Through the lateral extent of the lower blepharoplasty incision, both limbs of the lateral canthus, which have been freed from Whitnall’s tubercle by subperiosteal dissection, are purchased with two figure-of-eight, 30- gauge wire sutures (Fig. 4). To allow adequate upward mobility of the lateral canthus and lateral lid margin, it may be necessary to incise the lateral third of the scarred orbital septum with needle-tip electrocautery. The ends of each suture are twisted together, and then each twisted suture is passed from the lateral extent of the lower lid blepharoplasty incision along the lateral orbital rim to the lateral extent of the upper blepharoplasty (or coronal) incision. One twisted wire suture is passed from within the orbit through a drill hole placed 2 to 3 mm; the other twisted wire suture is placed approximately 5 mm beneath the zygomatico- frontal suture along the lateral orbital rim. These sutures are twisted to one another over the bridge of lateral orbital bone.:il:!- The canthus is elevated 2 to 3 mm above the level of the medial canthal plane. The amount of wire twisting will determine the amount of canthal elevation. The strand of four twisted wire ends is left approximately 0.5 cm long. This length allows the end to be placed into one of the drill holes to avoid its postoperative visibility or palpability. If the height of the lateral canthus needs readjustment postoperatively, the stump can be retrieved and twisted more to raise the canthus or untwisted to allow lower it.
Fig. 4. Technique of lateral canthopexy. (Above, left) Through the lateral extent of the lower lid blepharoplasty incision, the lateral canthus is identified and freed from Whitnall’s tubercle by subperiosteal dissection. (Above, right) The lateral canthus is purchased by two figure-of-eight, 30-gauge wire sutures. The ends of each wire suture are twisted together. (Below, left) Each set of twisted canthopexy wires is passed along the lateral orbit from the lower lid to the upper lid (or coronal) incision. To ensure adequate vertical mobility of the lateral canthus and lateral lid margin, it may be necessary to incise the lateral third of the scarred orbital septum. (Below, right) Each twisted wire suture is passed from within the orbit through drill holes made through the lateral orbital rim that were placed approximately 2 to 3 mm and 5 mm, respectively, beneath the zygomaticofrontal suture. The wire sutures are twisted to one another over the bridge of the bone. Passing the wire from inside to outside the orbit helps to apply the lid to the globe.
TemporaI Soft-Tissue Elevation
To ensure a smooth transition in the temporal area after midface elevation (avoiding the “Madame Butterflyâ€1 look), the temporal soft tissues are redistributed and elevated. If a bicoronal incision is used, a lateral brow lift will avoid any upper lid bunching after lateral canthal elevation. If temporal and upper lid incisions are used, an ellipse of skin is taken from t he lateral half of the upper lid to avoid upper lid redundancy.
Before soft-tissue closure, a suction drain is placed through a stab wound incision in the temporal scalp beneath the continuous composite soft-tissue flap. It is removed the following morning. Compressive dressings are avoided because they direct edema fluid toward the more distensible periorbital soft tissues. Figure 5 presents a schematic overview of the procedure.
RESULTS
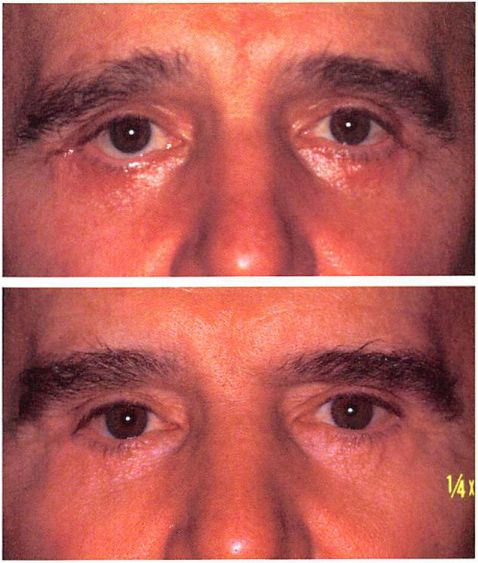
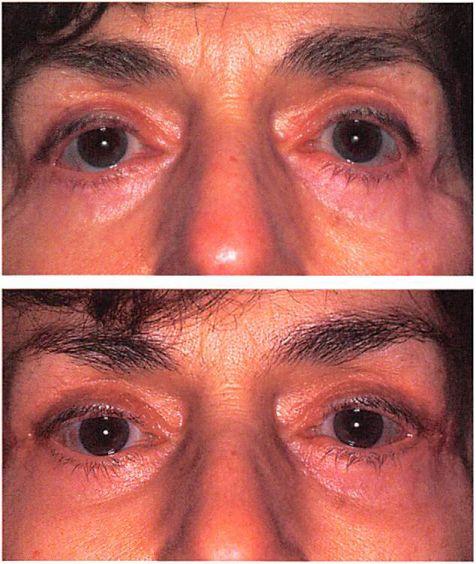
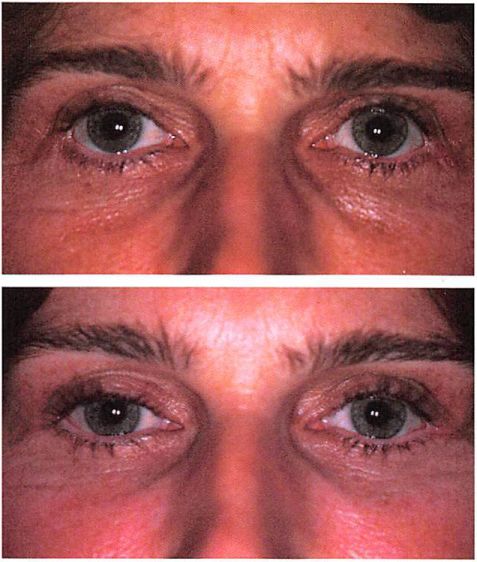
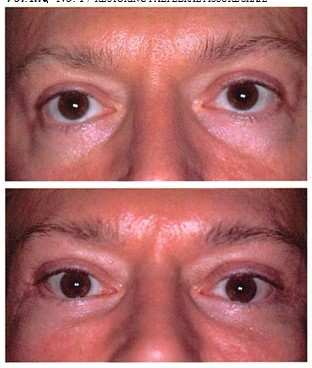
Lower lid position and palpebral fissure shape have been restored in a series of 15 patients operated on during a 6-year period (mean follow-up, 30 months). There were 12 women and three men, with an average age of 60 years (range, 42 to 68 years). The surgery was performed 2 months to 8 years after each patient’s last blepharoplasty. Three of the patients required revision of their canthopexy. One patient has a palpable canthopexy wire. The titanium screws are palpable if searched for but have not been objectionable. In eight of the patients who had complaints of dry eye, four had significant improvement and four had resolution of their symptoms. Clinical examples are shown in Figures 6 through 9.
DISCUSSION
Reproducible measurements have defined the shape of the palpebral fissure in youth, its changes with aging, and structures responsible for the change. Farkas et al.33 provided the average dimensions of the palpebral fissure in young adults. The fissure can be characterized as one that is long (medial to lateral canthal distance, 30.7 ± 1.2 mm) and narrow (upper lid margin to lower lid margin measured at midpupil, 10.8 ± 1.2 mm).
FIG. 5. Schematic ovemew of the procedure.
Fig. 6. A 60-year-old man who had undergone lace lilt, upper and lower lid blepharoplasty, and malar augmentation complicated by infection 15 years previously and a second rhytidectomy and lower lid blepharoplasty 3 months before corrective surgery. Midface elevation, lateral brow lilt, and lateral canthopexy were performed by bicoronal, lateral extent of lower blepharoplasty, and intraoral incisions. {Above) Preoperative appearance. {Below) Appearance 2 years postoperatively.
Several authors have documented changes in palpebral relations with aging. Shore found that the lower eyelid margin rested more inferiorly with increasing age (and increasing laxity).5 Ousterhout and Weil34 found that aging did not change the length of the lower lid margin as measured from canthus to canthus. Hill showed that there was a decrease in the width of the palpebral fissure with age. He also showed that the distance between the medial canthus and the punctum did not change with age.6 Neuhaus’7 measurements confirmed not only the persistent integrity of the medial canthus but also the deterioration of the lateral canthus. His measurements showed an increase in lateral orbital rim to lateral canthus distance in patients with senile ectropion. In summary, the shape of the palpebral fissure becomes more round with aging not because the horizontal length of the tarsal plate and lower lid margin increases, but rather because the lateral canthus migrates medially and the lower lid descends.
Fig. 7. A 69-year-old woman who had undergone rhytidectomy and upper and lower lid blepharoplasty 1 year and revision lower lid blepharoplasty 6 months before corrective surgery. Midface elevation, lateral brow lift, and lateral canthopexy were performed through bicoronal, lateral extent of lower lid blepharoplasty, and intraoral incisions. Surgery relieved dry eye symptoms. (Above) Preoperative appearance. (Beloxo) Appearance I year postoperatively.
These data are summarized in Figure 10. They provide both the morphologic and aesthetic rationale for lateral canthopexy as opposed to lid shortening procedures to maintain, improve, or restore lower lid position.
Ideally, lower lid rejuvenative procedures should improve lower lid contour without distorting the shape of the palpebral fissure.22 However, the literature and clinical experience indicate that many, if not most, patients who undergo lower lid blepharoplasty exchange a perceived improvement in lid contour for a change in the shape of their palpebral fissure. The most frequent complication after transcutaneous lower eyelid blepharoplasty is inferior malposition of the lid margin.8-11 Lisman et al.” contend that lower lid descent is so common after transcutaneous lower lid blepharoplasty, even in the face of minimal skin excision, that patients overwhelmingly have an increase in height of the palpebral fissure postoperatively: “Lower eyelid bowing is so common, even in the face of minimal skin resection,
Fig. 8. A 44-year-old woman who had undergone brow lift and bilateral upper and lower lid blepharoplasty 2 years before corrective surgery. A lateral brow lift, midface elevation, and lateral canthopexy were performed through bicoronal, lateral extent of lower lid blepharoplasty, and coronal incisions. (Above) Preoperative appearance. (Beloxo) Appearance 1 year postoperatively.
that it is not considered a complication if it does not produce a functional problem.†Newer operations designed to simultaneously rejuvenate the midface and lower lid have been accompanied by a significant incidence of clinically unacceptable palpebral fissure distortion. Patipa26 noted that many patients referred for postcosmetic lower eyelid retraction had undergone fat redraping in the course of their surgery. Both Hamra30 and Paul36 recently commented that the development and refinement of their combined lower lid and midface rejuvenation techniques have been accompanied by “painfulâ€35 or “steepâ€36 learning curves. Hester et al.3′ reported a 19 percent complication rate after using a trans-lower lid blepharoplasty approach for lower lid midface rejuvenation. Hamra35 advocates interdisciplinary rapport between plastic and oculoplastic surgeons for the “ever increasing number of patients with postoperative eyelid problems.â€
Fig. 9. A 46-year-old man who had undergone upper lid blepharoplasty, lower lid blepharoplasty, and malar miclface fat injections 18 months before corrective surgery. In addition to midface elevation and lateral canthopexy, the infraorbital rim was augmented with porous polyethylene implants (Yaremchuk, M.J. Infraorbital rim augmentation. Blast. Reconstr. Surg. 107: 1585. 2001) (Porex Surgical, Newnan, Ga.). This surgery was performed through temporal, intraoral, and lateral extent of upper and lower lid blepharoplasty incisions. Two revisional procedures were required to lower the position of the lateral canthus. {Above) Preoperative frontal and lateral appearance. {Below) Eight-month frontal and lateral appearance.
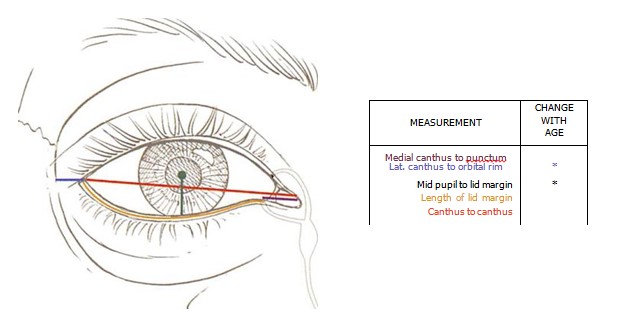
FIG. 10. Color-coded diagram showing how eyelid measurements change with aging. <->, no change; f , increases; | . decreases.
Transblepharoplasty midface rejuvenation procedures increase the number of variables the surgeon must control. These additional variables may include the stability of fixation of elevated midface soft tissues; orbicularis oculi muscle tone after the muscle is manipulated and potentially denervated when used as a source of lid support; fat viability when miniature flaps of intraorbital fat are draped over the infraorbital rim; shape of the lateral canthal angle after lateral canthotomy and canthoplasty; and outer lamellae adequacy after aggressive eyelid skin and muscle excision.
Fig. 11. {Left) Positive vector relationship: In the youthful face with normal globe-to-skeletal rim relations, the cheek mass supported by the infraorbital rim lies anterior to the surface of the cornea. The position of the cheek prominence beyond the anterior surface of the cornea is termed a positive vector. {Center) Negative vector relationship: In patients with maxillary hypoplasia, the check mass lies posterior to the surface of the cornea. The position of the cheek prominence beyond the anterior surface of the cornea is termed a negative vector. (For further explanation of positive and negative vector relationships, see Pessa, J. E., Desvigne, L. D., Lambros, V. S., Nimerick,J., Sugunan, B., and Zadoo, V. P. Changes in ocular globe-to-orbital rim position with age: Implications for aesthetic blepharoplasty of the lower eyelids. Aesthetic Plasl. Surg. 23: 337, 1999.) {Right) Reverscd- negative vector relationship: Alloplastic augmentation of the infraorbital rim can reverse the negative vector (Yaremchuk, M. J. Infraorbital rim augmentation. Rlasl. Reconstr. Surg. 107: 1585, 2001).
It is not surprising that procedures involving such extensive disassembly and reassembly of the lower lid, “the least forgiving structure involved in facial rejuvenation,often, if not usually, result in a palpebral fissure whose shape is different. To lessen morbidity associated with their transblepharoplasty approach, Hester et al.37 now decrease the amount of intralamellar manipulation, often release the lid structures from the skeleton from a remote lateral lid incision, use canthopexy rather than canthotomy and canthoplasty when possible, and stress secure fixation of elevated midfacial structures. These maneuvers and underlying concepts based on a large experience of pioneering aesthetic surgery and learned by the current author when treating posttraumatic cranial orbital deformities27-2” are very similar to those presented here for secondary aesthetic surgery. They are also similar to techniques previously described by the current author for primary cosmetic blepharoplasty and midface rejuvenation.24
Conventional transcutaneous blepharoplasty and transblepharoplasty approaches for midface rejuvenation do not directly violate the capsulopalpebral fascia or the conjunctiva. Only the lateral-most extent of these structures is incised when a wedge excision of the lower lid or a canthotomy and canthoplasty are performed. When traditional posterior lamellar spacer grafts are inserted to treat lower lid retraction, they are interposed between the lower border of the tarsal plate and the lower eyelid retractors. These grafts both separate the lid margin and tarsus from scarring and vertically splint the lid. Their violation of the posterior lamellae now introduces the unpredictability of the wound-healing process into all three of the lid lamellae. In addition, cartilage grafts introduce potential problems of buckling, thickness, and corneal irritation.38 The procedure described here preserves the integrity of these undamaged posterior lamellae. The lid margin is released from middle and outer lamellae scarring by en bloc subperiosteal release at the level of the orbital rim. The elevated lower lid position is maintained by filling the space between the scarred lid structures and orbital rim with the suborbicularis oculi fat.
The infraorbital rim and malar midface skeleton support the lower lid and midface soft tissues against gravitational descent. Patients with maxillary hypoplasia lack this support and are therefore considered “morphologically prone†to descent of the lower lid.39,40 These patients have an increase in the sagittal distance between the anterior surface of the globe and the infraorbital rim. Modifying the terminology of J elks and Jelks,41 Pessa et al.42 have defined a “positive vector†as the sagittal relation existing when the cheek prominence projects beyond the anterior surface of the cornea, and a “negative vector†as the cheek prominence lying behind the anterior surface of the cornea. In patients with maxillary hypoplasia (negative vector) presenting for correction of the palpebral distortion after previous lower blepharoplasty, the procedure presented in this article has been modified by first reversing the negative vector. With the addition of a small medially placed retroseptal transconjunctival incision, a porous polyethylene implant (Porex Surgical, Newnan, Ga.) is applied to the skeleton with titanium screws (Synthes Corporation, Paoli, Pa.) to augment the projection of the infraorbital rim and anterior maxilla43 (Figs. 9 and 11). Infraorbital rim augmentation not only provides structural support for the elevated and repositioned soft tissues, but it also improves aesthetics in this subset of patients with palpebral fissure distortion.
Michael J. Yaremchuk, M.D. Massachusetts General Hospital 55 Fruit Street, WACC 453 Boston, Mass. 02114-2696 myaremchuk@partners. org
ACKNOWLEDGMENTS
This study was supported by the Maxwell Blum Scholarship Fund.
REFERENCES
1. Shorr, N., and Fallor, M. K. “Madame Butterfly†procedure: Combined cheek and lateral canthal suspension procedure for post-blepharoplasty “round eye†and lower eyelid retraction. Ophthal. Plasl. Reconstr. Surg. 1: 229, 1985.
2. McCord, C. D., Jr., and Ellis, D. S. The correction of lower lid malposition following lower lid blepharoplasty. Plast. Reconstr. Surg. 92: 1068, 1993.
3. Baylis, H. I., Nelson, E. R., and Goldberg, R. A. Lower eyelid retraction following blepharoplasty. OphthaL Plasl. Reconstr. Surg. 8: 170, 1992.
4. Shagets, F. W., and Shore, J. W. The management of eyelid laxity during lower eyelid  blepharoplasty. Arch. Otolaryngol. Head Neck Surg. 112: 729, 1986.
5. Shore, J. W. Changes in lower eyelid resting position, movement and tone with age. Am. J. Ophthalmol. 99: 415, 1985.
6. Hill, J. C. An analysis of senile changes in the palpebral fissure. Can. J. Ophthalmol. 10: 32, 1975.
7. Neuhaus, R. W. Anatomical basis of “senile†ectropion. Ophthal. Plasl. Reconstr. Surg. 1: 87, 1985.
8. Edgerton, M. T., Jr. Causes and prevention of lower lid ectropion following blepharoplasty. Plast. Reconstr. Surg. 49: 367, 1972.
9. Hamako, C., and Baylis, H. I. Lower lid retraction after blepharoplasty. Am. J. Ophthalmol. 89: 517, 1980.
10. McCord, C. D., Jr., and Shore J. W. Avoidance of complications in lower lid blepharoplasty. Ophthalmology 90: 1039, 1983.
11. Lisman,R. D., Hyde, K., and Smith, B. Complications of blepharoplasty. Clin. Plasl. Surg. 15: 309, 1988.
12. Carraway, J. H., and Mellow, C. G. The prevention and treatment of lower lid ectropion following blepharo-plasty. Plast. Reconstr. Surg. 85: 971, 1990.
13. Patel, B. C. K., Patipa, M., Anderson, R. L., and McLeish, W. Management of postblepharoplasty lower eyelid retraction with hard palate grafts and lateral tarsal strip. Plasl. Reconstr. Surg. 99: 1251, 1997.
14. Baylis, H. I., Goldberg, P. A., and Groth, M. J. Complications of lower blepharoplasty. In A. M. Putterman (Ed.), Cosmetic Oculoplastic Surgery, 3rd Ed. Philadel-phia: Saunders, 1999. Pp. 429-456.
15. Smith, B., and Cherubini, T. S. Modifications of the Kuhnt-Szymanowski ectropion repair. In B. C. Smith (Ed.), Oculoplastic Surgery: A Compendium of Principles and Techniques. St. Louis: Mosby-Year Book, 1970.
16. McKinney, P. Use of tarsal plate resection in blepharoplasty on atonic lower lids. Plast. Reconstr. Surg. 59: 649, 1977.
17. Rees, T. D. Prevention of ectropion by horizontal shortening of the lower lid during blepharoplasty. Ann. Plast. Surg. 11: 17, 1983.
18. Hinderer, U. T. Blepharocanthoplasty with eyebrow lift. Plast. Reconstr. Surg. 56: 402, 1975.
19. Tenzel, R. R., Buffam, F. V., and Miller, G. R. The use of the “lateral canthal sling†in ectropion repair. Can. J. Ophthalmol. 12: 199, 1977.
20. Anderson, R. L., and Gordy, D. D. The tarsal strip procedure. Arch. Ophthalmol. 97: 2192, 1979.
21. Lisman, R. D., Rees, T., Baker, D., and Smith, B. Experience with tarsal suspension as a factor in lower lid blepharoplasty. Plasl. Reconstr. Surg. 79: 897, 1987.
22. Fagien, S. Algorithm for canthoplasty. The lateral retinacular suspension: A simplified suture canthopexy. Plast. Reconstr. Surg. 103: 2042, 1999.
23. Tsubota, K. Tear dynamics and dry eye. Prog. Relin. Eye Res. 17: 565, 1998.
24. Yaremchuk, M.J. Subperiosteal and full-thickness skin rhyudectomy. Plast. Reconstr. Surg. 107: 1045, 2001.
25. McCord, C. D., Jr. The correcuon of lower lid malposition following lower lid blepharoplasty. Plast. Reconstr. Surg. 103: 1036, 1999.
26. Padpa, M. The evaluation and management of lower eyelid retraction following cosmetic surgery. Plast. Re-constr. Surg. 106: 438, 2000.
27. Yaremchuk, M. J., and Kim, W. K. Soft-tissue alterations with acute, extended open reduction and internal fixation of orbital fractures./. Craniofac. Surg. 3: 134, 1992.
28. Yaremchuk, M. J. Orbital deformity after craniofacial fracture repair: Avoidance and treatment. J. Craniomaxillofac. Trauma 5: 7, 1999.
29. Phillips, J. H., Gruss, J. S., Wells, M. D., and Chollet, A. Periosteal suspension of the lower eyelid and cheek following subciliary exposure of facial fractures. Plast. Reconstr. Surg. 88: 145, 1991.
30. Stuzin,J. M., Wagstrom, L., Kawamoto, H. K., and Wolfe, S. A. Anatomy of the frontal branch of the facial nerve: The significance of the temporal fat pad. Plasl. Reconstr. Surg. 83: 265, 1989.
31. Whitaker, L. A. Selective alteration of palpebral fissure form by lateral canthopexy. Plast. Reconstr. Surg. 74: 611, 1984.
32. Flowers, R. S. Canthopexy as a routine blepharoplasty component. Clin. Plast. Surg. 20: 351, 1993.
33. Farkas, L. G., Hreczko, T. A., and Katie, M. J. Cranio facial norms in North American Caucasians from birth (one year) to adulthood. In L. G. Farkas (Ed.), An-thropometry of the Head and Face, 2nd Ed. New York: Raven Press, 1994. Appendix A.
34. Ousterhout, D. K., and Weil, R. B. The role of the lateral canthal tendon in lower eyelid laxity. Plast. Reconstr. Surg. 69: 620, 1982.
35. Hamra, S. T. Evaluation and management of lower eye lid retraction following cosmetic surgery (Discussion). Plast. Reconstr. Surg. 106: 454, 2000.
36. Paul, M. D. Morphologic and gender considerations in midface rejuvenation. Aesthetic Surg. J. 21: 349, 2001.
37. Hester, T. R., Jr., Codner, M. A., McCord, C. D., Nahai, F., and Giannopoulos, A. Evolution of technique of direct transblepharoplasty approach for the correction of lower lid and midfacial aging: Maximizing results and minimizing complications in a 5-year experience. Plast. Reconstr. Surg. 105: 393, 2000.
38. Baylis, H. I., Perman, K. I., Fett, D. R., and Sutcliff, R. T. Autogenous auricular cartilage grafting for lower eyelid retraction. Ophthal. Plast. Reconstr. Surg. 1:23,1985.
39. Wolfe, S. A, and Kearney, R. Blepharoplasty in the patient with exophthalmos. Clin. Plast. Surg. 20: 275, 1993.
40. Rees, T. D., and LaTrenta, G. S. The role of the Schirmer’s test and orbital morphology in predicting dry-eye syndrome after blepharoplasty. Plast. Reconstr. Surg. 82: 619, 1988.
41. Jelks, G. W., and Jelks, E. B. The influence of orbital and eyelid anatomy on the palpebral aperture. Clin. Plasl. Surg. 18: 183, 1991.
42. Pessa, J. E., Desvigne, L. D., Lambros, V. S., Nimerick,J.,Sugunan, B., and Zadoo, V. P. Changes in ocular globe-to-orbital rim position with age: Implications for aesthetic blepharoplasty of the lower eyelids. Aesthetic Plast. Surg. 23: 337, 1999.
43. Yaremchuk, M.J. Infraorbital rim augmentation. Plasl.Reconstr. Surg. 107: 1585, 2001.