Secondary Reconstruction of Posttraumatic Orbital Deformities
A retrospective analysis of our experience, techniques, and concepts for the secondary reconstruction of orbital injuries to 78 patients over a 15-year period is presented. Secondary orbital reconstruction has the following four basic steps: II) freeing of the overlying soft tissues by extensive subperiosteal dissection; (2) skeletal reconstruction, usually with onlay bone grafting and contour osteoplasty; (3) restoration of palpebral shape and position by medial and lateral canthopexy; and (4) soft-tissue refinement. Reconstruction required an average of at least two operations. In this series, there were no mortahties, three infections, and no reoperations for bleeding. Thirty patients required a second operation to an area previously addressed reflecting inadequacies in technique, the unpredictabihty of bone grafts, and soft- tissue scarring. Distortion of the skeletal infrastructure is most amenable to secondary reconstruction. Soft-tissue distortions that accompany bone malposition are less well corrected. Soft-tissue contraction is the limiting factor in successful reconstruction dictating separate movement of the overlying soft tissues and ligaments, their overcorrection, and subsequent revisional surgery. Secondary orbital reconstruction, although providing significant improvement, usually fails to restore the pre-injury appearance, and usually falls short of properly performed acute reconstruction.
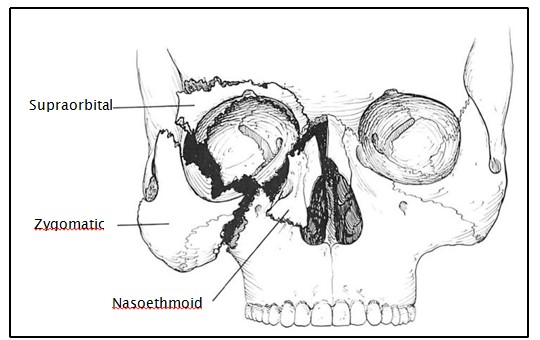
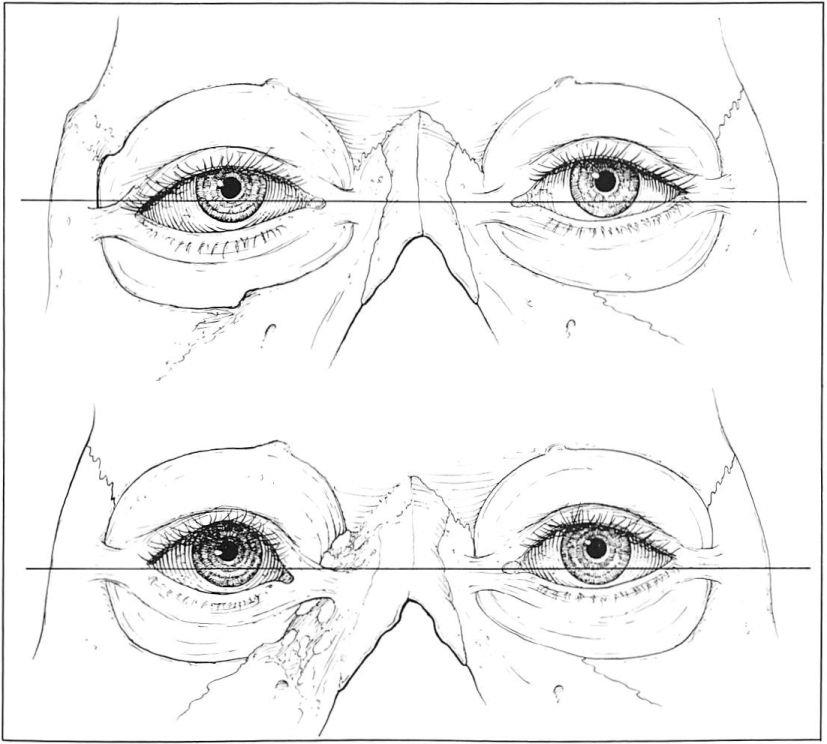
The boundaries of the orbit are defined by the supraorbital, nasoethmoidal, and zygomatic complexes (Fig 1). Certain untreated or inadequately treated orbital injuries may result in malposition of these complexes as well as subsequent distortion of the overlying soft tissue and the associated ligamentous structure of the eye (Fig 2). For these reasons, inadequate treatment not only results in contour deformity but also alterations in palpebral fissure shape and soft- tissue quality. Additionally, orbital displacement often results in a corresponding shift of the eye.
A fundamental truth of posttraumatic craniofacial reconstruction is that acute treatment affords the best opportunity to restore the preinjury structural relationships. Bone fragments too severely comminuted to be linked together must be replaced by bone grafts (1, 2]. Acute-phase treatment is generally possible up to about 3 weeks after trauma. After that, there is a gray time zone of several weeks before bone fragments become solidly fixed into position, so that they are moved only by osteotomy. Ultimately, soft-tissue healing becomes a dominant factor. The simultaneous and inseparable processes of scar formation and contraction resist repositioning of both bone and soft tissues. Reconstruction thus becomes secondary.
Secondary treatment of craniofacial trauma is possible based on principles evolved in craniofacial reconstruction [3-5]. Although highly predictable improvements can be expected, the results, in general, fall short of what would have been possible with primary treatment. This retrospective analysis presents our experience, techniques, and concepts that emerged from the secondary reconstruction of deformities resulting from injuries to these orbital complexes in 78 patients.
Clinical Experience
From 1972 to 1987, 78 patients presented for secondary reconstruction of posttraumatic orbital deformities. There were 36 males and 42 females. The average age was 23 years (range, 3-57 years); 53 patients, or more than two-thirds (68%), were between the ages of 16 and 30 years.
Seventy-six (97%) of these patients were injured by high-energy mechanisms; 61 (78%) being victims of motor vehicle accidents. Only 2 patients received their injuries in assaults. Forty-three (55%) of these patients suffered significant injuries to other organ systems.
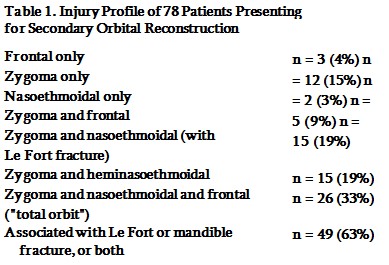
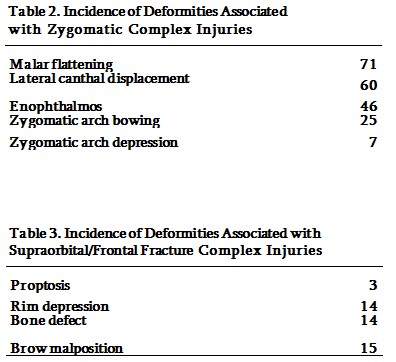
The initial bony orbital injury as determined by original radiographs (when available), operative reports, preoperative evaluation, and intraoperative findings during secondary reconstruction were classified as supraorbital, nasoethmoidal, zygomatic, or combinations thereof. Seventeen (22%) of the patients had injuries to one anatomical area, 35 (47%) had injuries to two areas, and 26 (33%) had injuries involving all three components or the entire circumference of the orbit. Forty-nine (63%) had associated Le Fort or mandibular fractures (Table 1). There was also a high incidence of associated ocular injuries. Twenty- six (33%) of the injuries were associated with blindness or significant loss of vision. Twenty-six patients (33%) had lacrimal dysfunction, and 28 (36%) had impaired ocular motility.
Fig 1. Orbit diagrammatically exploded into three common injury complexes, that is, supraorbital, nasoethmoidal, and zygomatic.
The average interval between the injury and the presentation for secondary reconstruction was 3 years and 8 months (2 months to 23 years). Almost one-half of the patients (46%) presented between 6 and 24 months after the injury. During the interval between injury and referral, an average of 3.3 operations (range, 0-20 operations) had been performed. Forty-six (59%) had 1 or 2 previous operations. Five patients had no attempts at reconstruction before referral.
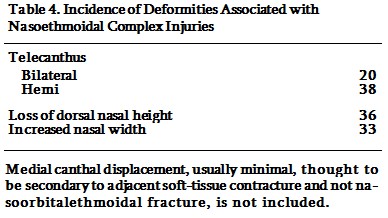
The contour, canthal, and soft-tissue deformities associated with inadequate initial therapy to each complex area have been previously described [6]. Their presence in any particular injury depends on its severity, the direction of impact, and the presence of adjacent accompanying injuries. The incidence of deformities associated with injury to each orbital complex area, that is, zygomatic, supraorbital, and nasoethmoidal, in this series, is presented in Tables 2, 3, and 4, respectively.
Treatment
Vision, visual fields, ocular motility, and lacrimal function were routinely evaluated by an ophthalmologist working closely with the plastic surgeon. Consultation by a neurosurgeon was obtained when frontal bone reconstruction was necessary.
Physical examination of the orbital complex focused on the position and symmetry of the skeletal and soft-tissue structures that provide its three- dimensional definition. Radiographic evaluation, when possible, included both plain radiographs and computerized tomographic (CT) scans; 8 x 10-inch
Fig 2. Relationship between ligamentous structures of orbit and their bony attachment. (Above) Displacement of the lateral wall of the orbit as seen in zygomatic complex fractures results in lateral canthal malposition and, usually, downward tilt of the palpebral fissure. (Below) Fractures of the nasoethmoidal complex result in lateral drift of the medial canthus, which is accompanied by some increase in the vertical and decrease in the horizontal dimension of the palpebral fissure.
photographs are helpful in preoperative planning and as a guide dining the operation.
Patients were closely questioned as to what they regarded as the most objectionable residuum of their injuries. It was clearly stated that previous appearance could hopefully be approximated but could almost never be fully restored.
Secondary orbital reconstruction required an average of at least two operations by us, at which time an average of four discreet areas were addressed. The first operation was the major one correcting as much of the structural foundations and attachments as possible. The average postoperative hospital stay after this initial procedure now averages 3 days.
Secondary orbital reconstruction involves the following four basic steps: (1) freeing of the soft tissues overlying the fracture sites; (2) skeletal reconstruction; (3) restoration of palpebral fissure shape; and (4) finally, soft-tissue refinement.
Exposure and Soft-Tissue Mobilization Access to the orbit was achieved by incisions placed through scars resulting from lacerations or previous incisions, or as is usually best, through a coronal incision (68% in this series). Besides having the advantage of leaving an inconspicuous scar, the coronal incision provides easy access for the harvest of cranial bone grafts. The orbital floor and anterior maxilla were approached through a lower blepharoplasty incision and skin muscle flap, or sometimes through a transconjunctival incision. All the soft tissues overlying the injured areas were then freed by subperiosteal dissection. It is important that the dissection is sufficiently extensive to release all soft tissues except at the optic foramen and infraorbital fissure, with damage to the lacrimal system carefully avoided.
Skeletal Reconstruction
Skeletal reconstruction attempts to restore three- dimensional contour as well as globe position. In our series, this was best accomplished with the use of onlay bone grafts, rather than with osteotomies. Cranial bone was usually the graft material of choice. Osteotomies are used to restore proper dental occlusion (4 patients in this series), or when large uncomminuted segments of bone exist intact after displacement.
Onlay bone grafting was performed to restore the projection of the lateral and inferior orbital rims, the malar prominence, and the nasal dorsum lish orbital shape and volume in an effort to restore eye position.
In certain select situations, synthetic material was used to restore skeletal contour. Implants specifically designed to augment the malar midface were used when there was no sinus exposure [7]. Proplast (Nova Med, Inc, Houston, TX) is ideal to fill out temporal depressions seen with temporal muscle malposition or atrophy.
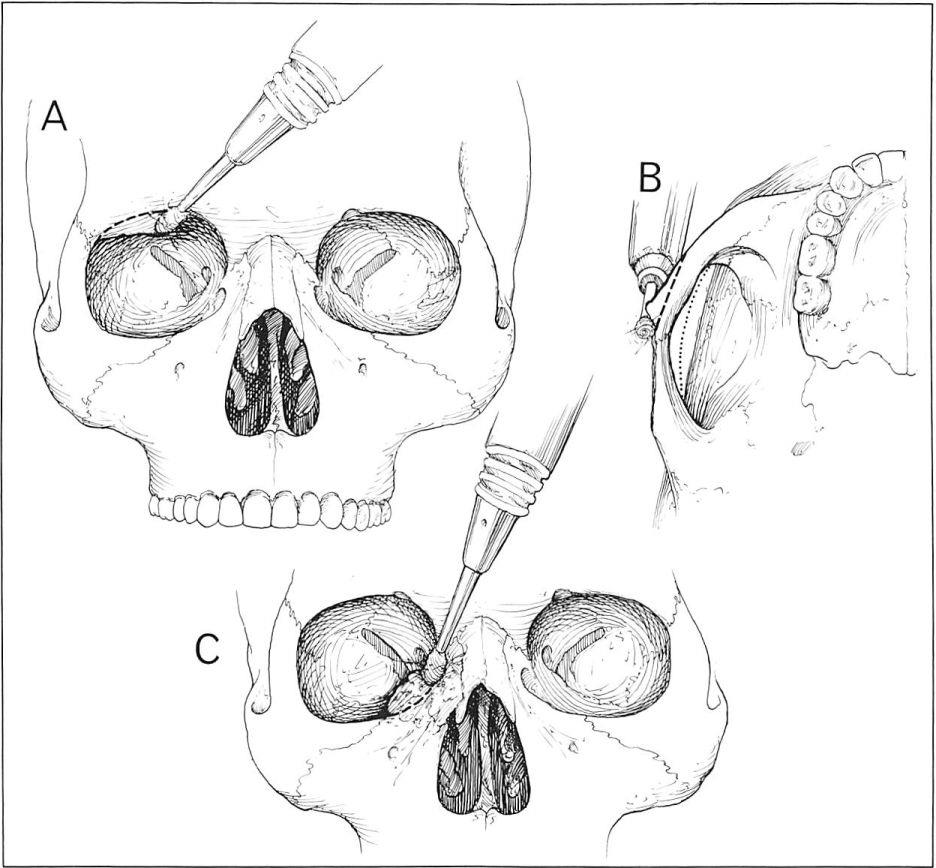
In areas where bone malposition results in abnormal prominences, bone contouring was used. Contouring was most often performed for the laterally bowed zygomatic arch, the inferiorly displaced supraorbital rim, and the widened nasal interorbital space area accompanying nasoethmoidal fractures (Fig 4) [8].
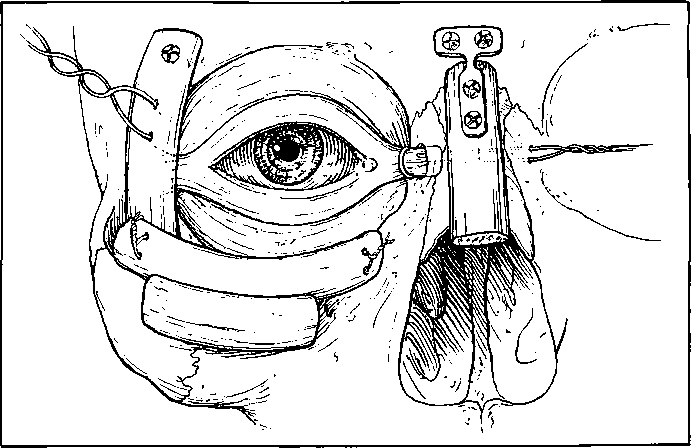
Restoration of Palpebral Fissure Shape Soft tissues were repositioned in a separate movement after extensive freeing from adjacent soft tissue and bone. Lateral and transnasal medial canthopexies (lateral, n = 72; medial, n = 47) were used to restore palpebral fissure shape (see Fig 3) by procedures previously described [9]. This procedure was often done in conjunction with upper and lower lid repositioning. Canthopexy was always performed with slight over-correction to allow for subsequent drift secondary to soft-tissue contracture [10].
Fig 3. Usual area where onlay bone grafts are placed to restore skeletal prominence together with completed medial and lateral canthopexies.
Soft-Tissue Refinement
Soft-tissue balance and contour was further restored by using various procedures. These procedures usually involved the revision of preexisting scars and restoration of soft-tissue bulk. Soft-tissue contour deformities were augmented by the use of pericranial flaps [11], dermisfat grafts [12], or small free muscle grafts.
In certain instances, facial symmetry was improved by operating on uninjured areas. For example, eyebrow level was sometimes adjusted at the time of coronal scalp flap closure. Appropriate shifts and excisions were made to raise or lower either brow. Similarly, upperlid skin excision, often on the uninvolved side, was sometimes done to balance the appearance of die supratarsal sulcus in patients with residual enophthalmus.
Results and Discussion
In this series, there were no mortalities, 3 infections, and no reoperations required for bleeding. Thirty patients required a second operation to an area previously addressed reflecting inadequacies in technique, the unpredictability in bone graft resorption time, and soft-tissue scarring. Because there is no available way to quantitate surface anatomy, it is impossible to scientifically evaluate the effects of surgery. Similar to those with other complex deformities, appearance or until it was clear that further surgery was not likely to add improvement. Adequate restoration of bone contour and ligamentous position was achieved in virtually all patients. The efficacy of soft- tissue reconstruction was more limited and related to the extent of the presenting deformity and to the amount of previous surgery.
Fig 4. Bone malposition that results in abnormal prominence may be contoured with a high-speed bun. The three most frequent areas are illustrated (A-C).
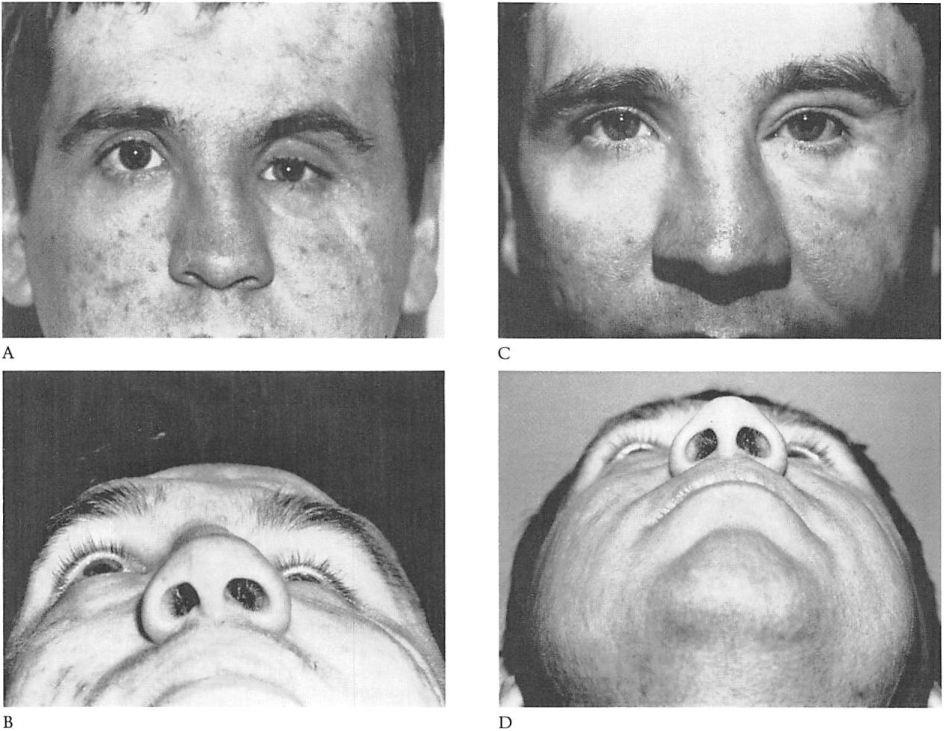
Reconstruction required several operations without a clear end point. Generally, the initial procedure was the major one, with subsequent procedures usually performed to obtain tissue refinement. The need for these operations evidently reflects a combination of the relative inadequacies in initial operative technique and judgment, and the unpredictability associated with bone graft resorption and soft-tissue contraction. Representative clinical cases are presented in Figures 5, 6, and 7.
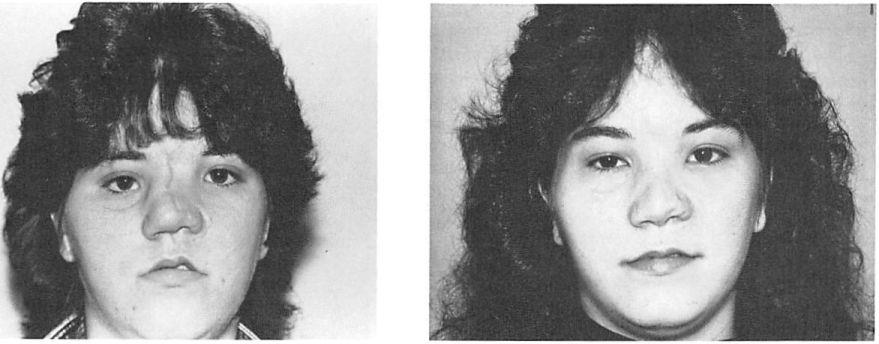
Fig 5. (A) Preoperative appearance of an 18-year-olcI woman who 6 months previously sustained a right zygomatic and nasoethmoid complex fracture treated elsewhere with open reduction. She has a flattened right malar prominence, bowed right zygomatic arch, and slight right enophthalmos. Both medial orbital walls are displaced laterally. The left alar base and upper lip are displaced with scar contracture. Using coronal and existing scars for exposure, cranial bone grafts were used to restore malar prominence and to reconstruct the right orbital floor and nasal dorsum. The zygomatic arch was reduced from lateral to medial and a lateral canthopexy was performed. Bilateral medial canthopexies and medial wall contouring plus soft tissue repositioning were done. (B) Twenty-two months after the major procedure described and a second soft-tissue repositioning procedure.
For secondary problems, following fracture lines as a guide for osteotomy has been advocated to correct posttraumatic zygomatic malposition [13-15]. Osteotomy seems most applicable in repositioning large segments of the frontal bone, lateral or supraorbital rim, or tooth-bearing segment. Lateral orbitotomy has been described to gain access deep into the orbit [16, 17) or to allow the lateral orbital rim’s anatomical repositioning [18]. In our experience, fracture comminution resulting from high-energy mechanisms made osteotomy and repositioning unnecessarily complicated, hence, we chose to add to or reduce the new posttraumatic bone infrastructure as necessary with onlay membranous bone grafts where possible [19] and with bone contouring. Screws and plates for bone fixation have been used more recently [2, 20-22], providing better immobilization and graft- recipient interface contact than conventional wiring techniques, perhaps resulting in better graft take and then volume persistence.
Enophthalmos, the posterior and usually inferior displacement of the eye, is a frequent finding. Recent volumetric and three-dimensional imaging studies [23-26] have shown that bony orbital enlargement accompanied by ligamentous displacement allows changes in soft-tissue shape and position. The treatment of enophthalmos required the extensive release of soft tissues from the walls of the orbit and repositioning by restoring the proper orbital volume with bone grafts, usually by placing bone behind the axis of the globe. In certain instances, camouflage was provided by filling the residual hollow of the supratarsal sulcus with small free-muscle or dermis grafts.
Proptosis resulting from supraorbital rim fractures is a relatively infrequent finding. This rim is more resistant to fracture than the adjacent facial bones [27]. Correction of this problem inevitably required an intracranial approach to reposition or contour bone fragments so the eye could return to its normal position and the orbital roof could be reconstructed.
Fig 6. (A, B) Preoperative appearance of a patient who, 1 year earlier, suffered a total orbit injury in a motorcycle accident. Emergency treatment addressed the intracranial injury only. Orbital reconstruction was attempted elsewhere 1 week and 1 month after injury at which time a Silastic implant was placed in the orbital floor. The patient has marked relrodisplacemenl of the supraorbital rim and zygomatic complex accompanied by marked enophthalmos and inferior globe displacement. (C, D) The patient is seen 6 months after fourth and final secondary procedure. The procedures included cranial bone graft reconstruction of the frontal defect, orbital floor, and lateral and inferior orbital rim. A lateral and medial canthopexy were also performed. Three subsequent soft-tissue and contouring procedures were done.
The shape and position of the palpebral fissure is largely determined by the position of the medial and lateral canthi [10, 28]. Displacement of the lateral wall of the orbit as seen in zygomatic complex fractures leads to lateral canthal malposition and, usually, downward tilt to the palpebral fissure. Fractures of the nasoethmoidal complex, unreduced, result in lateral drift of the medial canthus.
Our technique of transnasal medial canthopexy is similar to ones previously described [6, 18]. It may be a previously unreported added source of morbidity to the nasolacrimal system in those with nasoethmoid injuries. Patients with fractures of the nasoethmoidal complex have a 17% to 30% incidence of nasolacrimal obstruction after acute fracture treatment [28— 34], In this series, 21 patients who did not have symptoms of lacrimal obstruction after their initial therapy underwent medial transnasal canthopexy. Of this group, 7 patients (33%) developed lacrimal obstruction requiring dacryocystorhinostomy in 6 and lacrimal probing in 1 other.
The limiting factor in restoring the pr-injury appearance is the cumulative damage inflicted to the soft tissues. By providing the interface between the injuring object and the skeleton, the soft tissues actually receive more energy than the underlying bones [16]. Depending on the amount of energy absorbed, atrophy may occur at the point of impact while the energy-dissipating qualities of the soft tissue subject them to a penumbra effect of the scar forming process. If the underlying bone projection is maintained or restored after injury, the area of the overlying soft tissues is approximately maintained [1]. If the underlying bone prominence is lost, however, or if there is actual soft-tissue loss, wound contraction will result in reduction of some soft-tissue area and volume.
Fig 7. A young woman who suffered panfacial fractures treated elsewhere initially with intermaxillary hearframe fixation. A total of 15 secondary procedures were performed before presentation to us. (A) Preoperative view. Note the residual malposition of all orbital landmarks, that is, brow, medial and lateral canthi, globe position, and supratarsal sulcus. Patient is blind in the right eye. (B) Postoperative view. One year after major secondary procedure including contouring of medial orbits, right zygoma, cranial bone graft to nose, and bilateral medial and lateral canthopexies. ‘‘Hollow†temporal and malar areas were augmented with Proplast. The appearance remains limited by the abnonnal quality of the soft tissues.
Finally, it is important to recognize that the greatest number of these patients were managed without the benefit of CT scans, and the preoccupation with more severe or life-threatening injuries often precluded injury recognition and acute comprehensive treatment. Given these constraints, two-thirds of these patients had injuries to one of the orbital complexes unrecognized or thought sufficiently insignificant to warrant surgical therapy, only 2 patients had bone grafts during their acute reconstruction, no patient had three-point fixation of a zygomatic fracture, and only 1 patient with a nasoethmoidal complex injury had a transnasal canthopexy performed as part of the initial therapy.
Ideally, diagnostic and treatment modalities available to the plastic sturgeon today will allow primary care to be more complete. Precise, acute-phase, stable anatomical reconstruction of the facial skeleton will thereby allow the soft tissues to heal with minimum distortion and will subsequently minimize the need for secondary reconstruction.
References
1. Manson PN, Crawley WA, Yaremchuk MJ, et al: Midface fractures: advantages of immediate extended open reduction and bone grafting. Plast Reconstr Surg 76:1, 1985
2. Gruss JS, MacKinnon SE: Complex maxillary fractures: role of buttress reconstmction and immediate bone grafts. Plast Reconstr Surg 78:9, 1986
3. Tessier P: Total osteotomy of the middle third of the face for faciostenosis or for sequelae of Le Fort m fractures. Plast Reconstr Surg 48:533, 1971
4. Whitaker LA, Schaffer DB: Severe traumatic oculoorbital displacement. Plast Reconstr Surg 59:352, 1977
5. Wolfe SA: Application of craniofacial surgical precepts in orbital reconstmction following trauma and tumor removal. J Maxillofac Surg 10:212, 1982
6. Converse JM, Smith B, Wood-Smith D: Malunited fractures of the orbit. In Converse JM (ed), Reconstructive Plastic Surgery. Philadelphia, WB Saunders, 1977, pp 989-1040
7. Schultz RC: Supraorbital and glabella injuries. Plast Reconstr Surg 45:227, 1970
8. Whitaker LA: Aesthetic augmentation of the malar- midface structures. Plast Reconstr Surg 80:337, 1987
9. Whitaker LA, Pertschuk M: Facial skeletal contouring for aesthetic purposes. Plast Reconstr Surg 69:245, 1982
10. Whitaker LA: Selective alteration of palpebral fissure form by lateral canthopexy. Plast Reconstr Surg 74:611, 1984
11. Wolfe SA: The utility of pericranial flaps. Ann Plast Surg 1:146, 1978
12. Leaf N, Zarem H: Correction of contour defects of the face with dermal and dermalfat grafts. Arch Surg 105: 715, 1977
13. Freihofer HPM, Van Damme PA: Secondary posttraumatic periorbital surgery. J Maxillofac Surg 15:183, 1987
14. Perino KE, Zide MF, Kinnebrew MC: Late treatment of malunited malar fractures. J Oral Maxillofac Surg 42:20, 1984
15. Roncevic ML: Refracture of untreated fractures of the zygomatic bone. J Maxillofac Surg 11:252, 1983
16. Tessier P: Inferior orbitotomy—a new approach to the orbital floor. Clin Plast Surg 9:569, 1982
Manson PN, Ruas EJ, Iliff NT: Deep orbital reconstmction for correction of post-traumatic enophthalmus. Clin Plast Surg 14:113, 1987
18. Kawamoto HK: Late post-traumatic enophthalmus: a correctable deformity? Plast Reconstr Surg 69:423,1982
19. Zins JE, Whitaker LA: Membranous vs. endochondral bone: implications for craniofacial reconstmction. Plast Reconstr Surg 72:778, 1983
20. Jackson I, Somer P, Krar J: The use of Champy miniplates for osteosynthesis in craniofacial deformities and trauma. Plast Reconstr Surg 77:729, 1986
21. Manson PN, Soloman G, Pasker JP, et al: Compression plates in midface fractures. Plast Surg Forum 9:254,1986
22. Schilli W, Evers R, Niederdellmann H: Bone fixation with screws and plates in the maxillofacial region. Int J Oral Surg 10:329, 1981
23. Bite U, Jackson IT, Forbes GS, et al: Orbital volume measurements in enophthalmus using three-dimensional CT imaging. Plast Reconstr Surg 75:507, 1985
24. Manson PN, Clifford CM, Su CT, et al: Mechanisms of global support and post-traumatic enophthalmus: I. The anatomy of the ligament sling and its relation to intramuscular cone orbital fat. Plast Reconstr Surg 77:193, 1985
25. Manson PN, Givas A, Rosenbaum A, et al: Studies on enophthalmus: n. The measurement of orbital injuries and their treatment by quantitative computed tomography. Plast Reconstr Surg 77:203, 1985
26. Whitaker LA, Stalnecker MS, Katowitz JA: Secondary treatment of post-traumatic enophthalmus. In Marchac D (ed), Craniofacial Surgery. Proceeding of the Society of CranioMaxillo-Facial Surgery. Berlin, Springer-Verlag, 1987, p 467
27. Nahum AM: The biomechanics of maxillofacial trauma. Clin Plast Surg 2:59, 1975
28. Koomeef L: Sectional Anatomy of the Orbit. Amsterdam, Aeolus Press, 1981
29. Zide BM, McCarthy JG: The medial canthus revisited: an anatomical basis for canthopexy. Ann Plast Surg 11:1, 1983
30. Freihofer HPM: Experience with transnasal canthopexy. J Maxillofac Surg 8:119, 1980
31. Cruse CW, Blevins PK, Luce EA: Nasoethmoidorbital injuries. Trauma 20:551, 1980
32. Gruss JS: Nasoethmoidorbital fractures: classification and role of primary bone grafting. Plast Reconstr Sing 75:303, 1983
33. Stranc MF: The pattern of naso lacrimal and nasoethmoid injuries. Br J Plast Surg 23:339, 1970
34. Gruss JS: Frontonasoorbital trauma. Clin Plast Surg 9:577, 1982