Surgical Anatomy Relevant to the Transpalpebral Subperiosteal Elevation of the Midface
Abstract
Background: The surgical anatomy of the midface relevant to its subperiosteal elevation and repositioning is assessed.
Objectives: The aim of this study is to give more details on the anatomy relevant to the midface lift. Methods: Twenty hemifacial dissections were performed. The location of the zygomatic branches of the facial nerve (ZBFN) and the terminal branches of the infraorbital nerve (ION) were dissected. The location of the masseteric and zygomatic ligaments and the elevation of midface following their release were documented.
Results: On average, there were 3 branches of the facial nerve innervating the zygomatic major muscle and 1.8 branches entering the muscle superior to the caudal origin of the zygomaticomaxillary (ZM) suture. The most superior ZBFN was found to lie at an average of 6.2±1.6 mm cranial to ZM suture and 1.4±0.4 mm superï¬cial to the bone. The most inferior branch was at a mean of 4.8±3.3 mm inferior to ZM suture. On average the ION had 5.2 branches that traveled for 10.2 mm above the periosteum before they passed into a superï¬cial plane. Division of the zygomatico-masseteric retaining ligaments allowed forelevation of the midface by 4.8±1.0 mm medially and 5.5±.9 mm laterally.
Conclusions: Branches of the ZBFN and ION lie in close proximity to the subperiosteal plane in the midface. These branches are at risk for damage during release of the upper zygomatic ligaments and placement of the periosteal suspension sutures during midface elevation procedures.
Accepted for publication November 11, 2014.
Midfacial aging is characterized by ptosis of the cheek skin and descent of the attenuated lower eyelid skin below the inferior orbital rim, which lengthens the lower eyelid and obliterates the palpebro-malar junction.1 Additionally, the malar fat pad descends resulting in loss of malar prominence, the tear trough becomes hollower, and the nasolabial folds deepen. 2 In 1996, Hester, Codner, and McCord published the centrofacial approach for correction of facial aging by means of the transblepharoplasty subperiosteal cheek lift. 3This technique and its subsequent modiï¬cations4, 5were designed to correct midfacial aging by a central direct approach, allowing the vertical elevation of the midface by suspending the subperiosteal cheek flap to the orbital rim. 2
Although this technique is generally considered safe and low complication rates have been reported, 6primary structures could be damaged during the dissection and placement of anchoring sutures, namely the zygomatic branches of the facial nerve (ZBFNs) and the infraorbital nerve (ION). This study was performed to provide a focused and detailed description of the relative position and course of the terminal branches of the ION and ZBFNs in relation to the underlying skeletal landmarks and retaining ligaments of the midface.
Facial Surgery
METHODS
Twenty fresh hemifaces from 10 cadavers were dissected with 3.5× magniï¬cation. The bodies were donated to the Cleveland Clinic Body Donation Program. This study was Institutional Review Board exempt, because anatomical study was performed on bodies donated for research purposes. In 16 hemifaces, the branches of the facial and ION were dissected (8 hemifaces foreach nerve). In 4 hemifaces the subperiosteal face lift was performed, and the elevation of the soft tissue was checked before and after the release of the zygomatic cutaneous and upper masseteric cutaneous ligaments.
Facial Nerve Dissection
The superior extent of the superï¬cial musculo-aponeurotic system (SMAS) incision was at the level of the upper border of the zygomatic arch. Sub-SMAS dissection proceeded from lateral to medial, remaining superï¬cial to parotidomasseteric fascia. Once the zygomatic major muscle was identiï¬ed, the muscle was dissected medially along its superï¬cial belly. The distal zygomatic and buccal facial nerve branches were exposed and dissected anterograde. A superï¬cial parotidectomy was performed revealing the entire course of the zygomatic and buccal facial nerve branches.
Infraorbital Nerve Dissection
An upper gingivo-buccal sulcus incision was performed. The anterior maxilla and zygomatic body were dissected subperiosteally. The origins of the upper masseteric and the zygomatic cutaneous ligaments were exposed. The inferior orbital nerve was identiï¬ed and protected. A transconjunctival incision was performed in the lower eyelid, and the dissection was performed in the preseptal plan down to arcus marginalis. The subperiosteal plane was entered and the dissection proceeded medially and laterally preserving the ION. The periosteum at the foramen was divided and the nerve fascicles were followed in the supraperiosteal plane until they started to cross to a more superï¬cial plane.
Midface Elevation A transconjunctival incision was performed in the lower eyelid and the dissection was performed in the preseptal plan down to arcus marginalis. The subperiosteal plane was entered and the dissection proceeded medially and laterally preserving the ION.
An upper gingivo-buccal sulcus incision was then performed. The anterior maxilla and zygomatic body were dissected subperiosteally. The origins of the upper masseteric and the zygomatic cutaneous ligaments were exposed and released. Two 4/0 Ethibond sutures were placed in the periosteal layer, 3 cm inferior to the pupil and lateral canthus, which corresponds to the level of the malar fat pad prominence. Traction was applied to test the elevation of the soft tissues in reference to the pupil and lateral canthus. The upper masseteric and zygomatic cutaneous retaining ligaments were then released and traction was reapplied to assess for the elevation of the malar fat pad.
Measurements
Each hemi-face was marked with vertical (y) and horizontal (x) coordinates. The horizontal axis was deï¬ned as a straight line extending from the upper margin of the tragus to the infraorbital rim, corresponding to the Frankfort horizontal line. The vertical axis started from the upper border of the tragus and extended inferiorly perpendicular to the x-axis. A measuring tape was placed along each axis, parallel to them, and curved to conform to the curvature of the facial skeleton, as previously published.7 The following data were obtained for the ZBFN: (1) the number of ZBFN in relation to the zygomatic major muscle, (2) the distance of the ZBFN from the tragus, (3) the distance of the ZBFN branches from the zygomatico-maxillary bone, and (4) the position of the ZBFN on a vertical axis from the inferior border of the zygomatic maxillary buttress as they pass underneath the lateral border of the zygomatic major muscle (positive numbers indicated superior branches and negative numbers indicated inferior branches to the inferior border of the zygomatic maxillary buttress). The measurements regarding the ION included: (1) the distance between the infraorbital foramen and the infraorbital rim; (2) the number of the terminal branches of the ION; (3) the distance the ION branches traveled above the periosteum before entering into a more superï¬cial plane, measured from the infraorbital foramen. The elevation of the midfacial soft tissues before and after release of the zygomatico-facial and maxillary retaining ligaments was measured as follows: 2 dots were tattooed on the cheek skin 3 cm from the pupil (medial measurement) and the lateral canthus (lateral measurement) prior to the midface dissection. The distance between the marked points and the pupil and lateral canthus was measured prior to and following release of the zygomatic and upper masseteric ligaments, while applying constant pressure on the suspension sutures. Of note, the same operator performed all the dissections and measurements.
RESULTS
There were 5 males and 5 females. The average age was 57 years (range, 47-71 years), and the average body mass index was 28 (range, 24-32). None of these cadavers had under gone previous surgery on the face.
Zygomatic Branches of the Facial Nerve
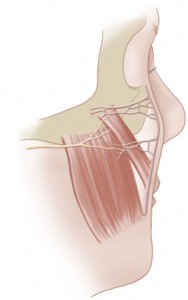
On average, there were 3 branches of the facial nerve innervating the zygomatic major muscle (upper, middle, and lower) and 1.8 branches entering the muscle superior to the caudal border of the ZM suture. The upper ZBFN was found to lie at an average of 6.2±1.6 mm cranial to the inferior border of the ZM suture, 6.4±0.4 mm from the tragus, and at 1.4±0.4 mm of elevation from the bone. The middle branch was at a mean of 2.3±4.2 mm cranial to the inferior border of the ZM suture, 6.9±0.3 mm from the tragus, and at 1.3±0.4 mm of elevation from the bone. The lower branch laid at a mean of 4.8±3.3 mm inferior to the caudal border of the ZM suture, at an average of 7.2±0.1 mm from the tragus (Figure 1). The lower branch did not overlie the bone.
Infraorbital Nerve
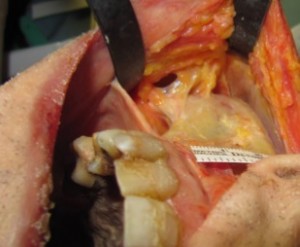
ION emerged from the infraorbital foramen at an average of 9.4±1.8 mm from the infraorbital rim. After the exit from the foramen, the nerve divided into an average of 5.2 branches: lower eyelid, malar, medial upper lip, lateral upper lip, and lateral cheek (Figure 2A). Occasionally, a second malar branch was present (14%). The terminal branches of the ION traveled above the periosteum before they passed into a superï¬cial plane (Figure 2B).
The lower eyelid branch had the shortest supraperiosteal course(averaging 5.9±1.2 mm), followed by the malar branch and lateral cheek branches that entered the subcutaneous layer at a mean of 8.0±2.2 mm and 9.9±3.4 mm, respectively. The medial and lateral upper lip branches traveled an average of 12.6±2.2 mm and 12.2±2.1 mm before becoming superï¬cial (Figure 3).
Zygomatic Cutaneous and Upper Masseteric Cutaneous Ligaments
These ligaments represented a continuous row of dense and stout fibers originating from the anterolateral aspect of the maxillary buttress, upper anterior masseteric muscle, and zygomatic body (Figures 4 and 5). Soft tissue elevation under traction, prior to division of the retaining ligaments, averaged 4.1±0.5 mm medially and 4.4±0.6 mm laterally (Supplementary Video S1). Following the release of the zygomatic and masseteric ligaments, the elevation of the malar fat pad and overlying soft tissues increased 4.8±1.0mm medially and 5.5±.9 mm laterally (Supplementary Video S2).
DISCUSSION
Transpalpebral subperiosteal midfacelift is a powerful technique in facial rejuvenation. The transconjunctival access to the midface avoids the need for extensive peripheral to central intermediate plane dissection Application of the vertical vector allows restoration to a youthful midface and lower lid contour without the lateral sweep. In addition, the vascular supply to the face is not significantly reduced allowing for concomitant skin rejuvenation.1 We prefer the transconjunctival incision because it avoids the delamination and relamination of skin muscle flaps, which increase the risk of subsequent lower lid malposition.8 This technique, which does not leave visible scars, consists of a combination of transconjunctival and transbuccal subperiosteal dissections to achieve complete release of the orbitomalar, zygomaticofacial, and upper masseteric ligaments.6 The transbuccal approach is essential to release the ligamentous attachments and allows for effective redraping and upward mobilization of the lower eyelid and premalar soft tissues, which are then suspended to the inferior orbital rim. Although the subperiosteal dissection provides protection of the terminal branches of the fifth and seventh cranial nerve, these structures are in danger during both placement of deep suspension sutures and release of the osteocutaneous ligaments. The focus of the majority of studies published previously was the localization of the important midfacial structures in the superficial to deep axis, an approach more relevant to the traditional facelift. In the current study, we evaluated the course of the same anatomical structures in a conversely deep to superï¬cial axis to facilitate locating them during the subperiosteal midface lift. The zygomatic cutaneous ligaments are strong ï¬bers that originate at the inferior border of the zygomatic arch and extend anteriorly to the junction of the arch and body of the zygoma.9 Mendelson et al10-12 described zygomatic ligaments medial to the junction of the arch and body, located along the origins of the facial expression muscles (the zygo maticus major, zygomaticus minor, and levator labii superioris). The masseteric cutaneous ligaments arise from the masseteric fascia over the masseter muscle.13,14
Figure2. Infraorbital nervefascicles run on the anteriormaxillary periosteum afterexiting the infraorbital foramen (A)of a 64-year-oldfemale cadaver, andinfraorbital nerve(ION) fascicles areshown entering the subcutaneoustissues (B). Thearrows indicate the point ofelevation from the periosteum
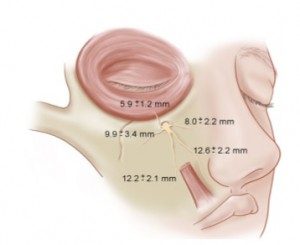
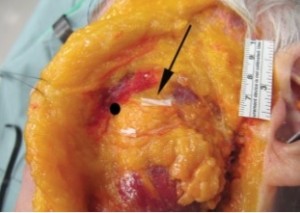
Figure4. Masseteric cutaneous ligaments of a 52-year-old male cadaver:stout ï¬brous ligament origin from the maxillary buttress and the anterior margin of masseter muscle.
Whereas in some anatomic studies, researchers have shown the ligaments arising along the anterior border of the masseter,13,14 others have shown them to arise 1 to 2 cm posterior to the anterior border,15 and even from the middle portion of the muscle.16 Our dissections confirmed the origin of stout masseteric ligaments both from the periosteum of the maxillary buttress and the anterior masseteric fascia, and that their release allowed an average elevation of the midfacial soft tissues of 4.8±1.0 mm medially and 5.5±.9 mm laterally. These ligaments are 2 different structures and are important landmarks for the zygomatic and buccal branches of the facial nerve.17 Alghoul and Zins7 showed that the upper zygomatic nerve passed 4 mm deep to the deep fascia between the main zygomatic and upper masseteric ligaments, and that the lower zygomatic nerve passed inferior or penetrated the upper masseteric ligament. These findings were confirmed by our dissections, which in addition revealed that the upper and middle ZBFNs travelled 1.4±0.4 mm and 1.3±0.4 mm superficial to the zygomatico-maxillary bone. The release of these ligaments is absolutely necessary to allow repositioning of the malar mound; however, because of the proximity of these branches to the periosteum at the level of the zygomatico-maxillary suture, caution should be exercised in generous application of electrocautery during the release of the retaining ligaments to avoid injury to the periosteum and the facial nerve.
The superior branches of the facial nerve innervating the zygomatic major muscle could be injured during elevation or suspension. However, given the redundancy in the innervation of the muscle, such injury is highly unlikely to have a detrimental effect on the muscle, because it will remain innervated by the inferior branches. This partial sacriï¬ce of facial nerve branches innervating the zygomatic major has been demonstrated with facial reanimation procedures, when sacrificing 1 or 2 branches to the zygomatic major result in minimal functional consequences. However, as a limitation common to any anatomical study, the clinical relevance of damage to one of the ZBFNs could not be assessed. Rashcke et al identified a safe zone of dissection in the midface to minimize injury to the ION employing skeletal and dental landmarks to locate the infraorbital foramen.18 However, the ION could be damaged not only at its exit from the foramen, but also along its long supraperiosteal course. The ION emerges from the infraorbital foramen and runs above the periosteum between 5.9±1.2 mm (branch to lower eyelid) and 12.2±2.1 mm (branches to upper lip) prior to entering the subcutaneous soft tissue. The lower branches of the ION, because of the longer supraperiosteal course and thinness of the periosteum in this area, are susceptible to inadvertent injury during the placement of the suspension sutures. Sensory loss in the territory of the ION, although rare, has been reported (6.4%)19,20 and can be avoided by remaining cognizant of the course and position of the terminal branches of the ION. Weakness of the branches of the facial nerve after midface lift has been reported in 1% of the patients.20 For the above reasons we place 2 sutures radially (parallel to the course of the fascicles) at 13 and 22 mm lateral to the infraorbital foramen, and we avoid deep passage of the suture through the periosteum to decrease the chance of inadvertent injury to the ION. Sutures placed more than 13 mm from the ION are considered safe.
CONCLUSIONS
Branches of the ZBFN and ION lie in close proximity to the subperiosteal plane in the midface. These branches are at risk for damage during release of the upper zygomatic ligaments and placement of the periosteal suspension sutures during midface elevation procedures. Recognition of this surgical anatomy is also important during the placements of implants for midface augmentation.
Supplementary Material
This article contains supplementary material located online at www.aestheticsurgeryjournal.com.
The zygomatic branch of the facial nerve(ZBFN) runs in close proximity to the upper massteric and zygomatic ligaments and can be damaged when releasing these ligaments from their skeletal attachments.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no external financial support for the research, authorship, and publication of this article.
REFERENCES
- Hester T, Codner M, MacCord C, et al. Transorbital lower-lid and midface rejuvenation. Operat Tech Plast Reconstr Surg. 1998;5(2):163-184.
- Hester TR Jr., Codner MA, McCord CD, et al. Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: Maximizing results and minimizing complications in a 5-year experience. Plast Reconstr Surg. 2000;105(1): 393-406; discussion 407-408.
- Paul MD, Calvert JW, Evans GR. The evolution of the midface lift in aesthetic plastic surgery. Plast Reconstr Surg. 2006;117(6):1809-1827.
- Hester T, Codner M, McCord C. The centro facial approach for correction of facial aging using the transblepharoplasty subperiostealcheeklift.AesthetSurgJ.1996;16:51.
- Paul MD. An approach for correcting mid facial aging with aperiostealhingeflap.AesthetSurgJ.1997;17(1):61-63.
- SeitzI A,LlorenteO,FewJW.The transconjunctival deep plane midface lift: A 9-yearexperienceworking under the muscle. Aesthet SurgJ.2012;32(6):692-699.
- Alghoul M, Bitik O, McBride J, et al. Relationship of the zygomatic facial nerve to the retaining ligaments of the face: The sub-SMAS danger zone. Plast Reconstr Surg. 2013;131(2):245e-252e.
- Yaremchuk M J. Subperiosteal and full-thicknessskin rhytidectomy. Plast Reconstr Surg. 2001;107(4):1045-1058.
- Mitz V, Peyronie M. The superï¬cial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58(1):80-88.
- Mendelson BC, Muzaffar AR, Adams WP Jr. Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg. 2002;110(3):885-896;discussion 897-911.
- Mendelson BC. SMAS ï¬xation to the facial skeleton: Rationale and results. Plast Reconstr Surg. 1997;100 (7):1834-1842; discussion 1843-1845.
- Mendelson BC. Surgery of the superï¬cial musculoaponeurotic system: Principles of release, vectors, and ï¬xation. Plast Reconstr Surg. 2001;107(6):1545-1552; discussion 1553-1555, 1556-1557, 1558-1561. 13. Stuzin JM, Baker TJ, Gordon HL. The relationship of the superï¬cial and deep facial fascias: Relevance to rhytidectomy and aging. Plast Reconstr Surg. 1992;89(3):441-449; discussion 450-451.
- Stuzin JM, Baker TJ, Gordon HL, et al. Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg. 1995;22(2):295-311.
- Mendelson BC. Extended sub-SMAS dissection and cheek elevation. Clin Plast Surg. 1995;22(2):325-339.
- Ozdemir R, Kilinc H, Unlu RE, et al. Anatomicohistologic study of the retaining ligaments of the face and use in face lift: Retaining ligament correction and SMAS plication. Plast Reconstr Surg. 2002;110(4):1134-1147; discussion 1148-1149.
- Alghoul M, Codner MA. Retaining ligaments of the face: Review of anatomyandclinical applications.Aesthet Surg J. 2013;33(6):769-782.
- Raschke R, Hazani R, Yaremchuk MJ. Identifying a safe zone for midface augmentation using anatomic landmarks for the infraorbital foramen. Aesthet Surg J. 2013;33(1):13-18.
- Finger ER. A 5-year study of the transmalar subperiosteal midface lift with minimal skin and superï¬cial musculoaponeurotic system dissection: A durable, natural appearing lift with less surgery and recovery time. Plast Reconstr Surg. 2001;107(5):1273-1283; discussion 1284.
- Finger ER. Transmalar subperiosteal midface lift: Technical modiï¬cations, new suggestions, and limitations. Aesthet SurgJ.1998;18(3):222-225.


Leave Comments
You must be logged in to post a comment.