Surgical Techniques
The order of procedures is (1) upper lid blepharoplasty, (2) subperiosteal brow and midface lift, (3) lower face lift, and (4) lower lid blepharoplasty.
Upper Lid Blepharoplasty
Because the lateral brow lift removes considerable lateral upper lid skin redundancy, lid skin excision is conservative. Less upper lid skin is removed than when an upper lid blepharoplasty is done as an isolated procedure. A medial fat pocket bulge is usually the primary target during upper lid fat removal. Care is taken to avoid over resection of  fat.
Brow and Midface Lift
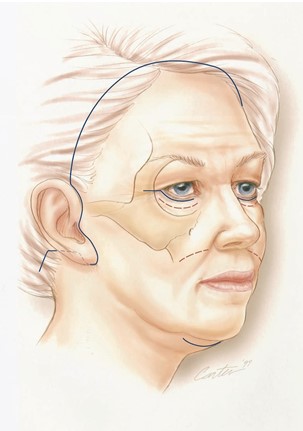
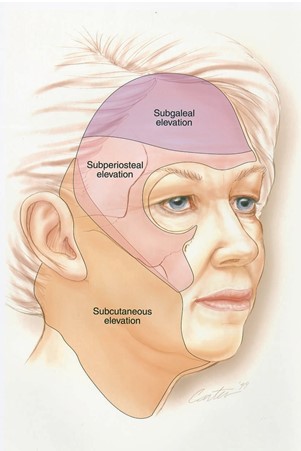
The brow and midface lift are performed using bicoronal and intraoral incisions (Fig. 6) to allow separation of the soft tissues from the facial skeleton, similar to the techniques advocated for the skeletal exposure necessary for complex midface and orbit repair.18 Through the bicoronal incision, the scalp is elevated away from the skull in first a subgaleal and then, at approximately 2 cm above the supraorbital rim, a subperiosteal plane (Fig. 7). In the temporal area, the superficial layer of the deep temporal fascia is incised at the level of the zygomaticofrontal suture to expose the superficial temporal fat pad.19 Dissection is carried along the surface of the superficial temporal fat pad until the zygomatic arch is reached. Its periosteum is incised and elevated. From the intraoral approach, subperiosteal dissection extends laterally from beneath the infraorbital nerve foramen over the lateral maxilla and the masseter muscle to connect with the dissection from above. Notably, the lateral canthus  and  arcus marginalis remain attached to the zygoma.
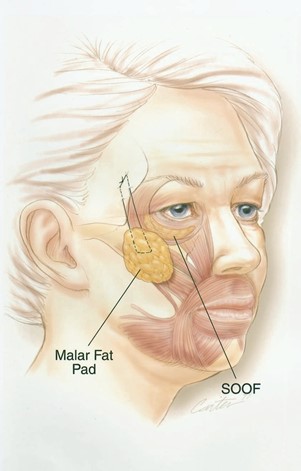
After the subperiosteal dissection, the cheek soft-tissue mass should be mobile. Pre-operatively, a point is marked approximately 3 cm beneath the lateral canthus. This point is transferred to the subperiosteal surface of the cheek flap by passing a straight needle through the full thickness of the flap. Through the intraoral incision, the needle tip is visualized and the point of penetration is purchased with a figure-of-eight 2-0 polyglycolic acid suture. Through the coronal access, the stitch is used to elevate the cheek tissues vertically. This elevation is stabilized by suturing to the deep temporal fascia at the level of the zygomatico- frontal suture (Fig. 8). A second elevation/ fixation stitch is placed usually 1 cm more medially, both for security and individualized impact on more medial cheek elevation. A suction catheter is placed over the maxilla, zygoma, and temporal area and exits through a stab wound incision in the temporal scalp. It is removed the morning after  surgery.
Lower Rhytidectomy
The coronal incision is continued preauricularly, then retrotragally, around the lobule, above the postauricular sulcus and just above the level of the lateral canthus and tragus back into the scalp (Fig. 6). A submental incision is also made. Through this access, a full-thickness skin subcutaneous flap is elevated on the superficial musculoaponeurotic system (SMAS)- platysma anatomic continuum20 (Figs. 9, 10). The extent of medial dissection increases as one proceeds from the temporal area into the neck. In the temporal area, a biplanar flap is created—subperiosteal and subcutaneous. This area of dissection overlap is approximately 2 to 3 cm and extends inferomedially toward Stenson’s duct (Fig. 7).
The subcutaneous dissection allows identification of the lateral aspect of the orbicularis oris muscle, divides the mandibular retaining ligaments,21 and is carried across the midline in the neck. Inferiorly, dissection is carried just beneath the hyoid.
This plane of dissection is most easily identified by identifying the posterior edge of the platysma muscle where it abuts onto the sternocleidomastoid muscle. One can follow this muscle medially and superiorly. All dissection is done with scissors under direct visualization. With little exception, each vessel that penetrates the platysma can be identified, allowing its coagulation with bipolar cautery before it is divided.
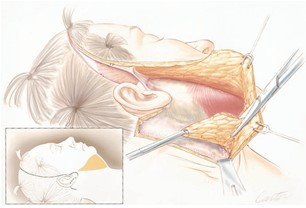
Submental and submandibular contouring.  After the flaps are elevated, a submental lipectomy is performed by removing fat with scissors directly from the under surface of the full-thickness skin-subcutaneous flap (Fig. 9). This is routinely done in the submental and jowl area. It is unusual for the surgeon to remove any sub- platysmal fat.
Management of the platysma is  determined by its anatomy.22 Most often, mandibular con- tour is accentuated by creating a modified platysma L-flap. At the level of the hyoid, a 2- to 2.5-cm wedge of platysma is excised. Laterally, the platysma is separated from the border of the sternocleidomastoid muscle for approximately 1 to 2 cm, then resuspended laterally where it is sutured to the sternocleidomastoid fascia just lateral to the postauricular nerve.23 Above the mandible, the continuation of platysma, now the SMAS, may become redundant because of the platysma suspension. For that reason, the SMAS may be imbricated or excised, depending on its redundancy, to improve the contour of the face in this area. Ptotic submandibular glands are managed using Feldman’s corset technique directly over the gland.24
Redraping of flaps. The coronal and face lift flaps are redraped and tailored. In general, maximum tension is placed superolaterally on the lateral brow, allowing 2 to 3 cm of scalp to be excised. Approximately 1 cm of scalp is excised in the midline. Skin flaps are redraped with vertical elevation in the temporal area and superolateral tension behind the ear. A total of 2 to 4 cm of skin is routinely removed from behind the ear. Suction drains are placed in the neck.
Lower Lid Blepharoplasty
The desired lower lid contour is achieved by a combination of fat excision, if necessary, skin redistribution, and tailoring. When fat protrusion is prominent, the transconjunctival retroseptal approach is used to excise the fat that protrudes beyond the infraorbital rim. Redundant eyelid skin is managed by first making an incision approximately 1 mm beneath the lash line. The skin is then separated from the underlying orbicularis oculi muscle for approximately 10 to 12 mm and redraped. It may be necessary to trim the surface of the muscle or imbricate it with absorbable sutures to optimize the contour. A total of 1 to 3 mm of skin is excised.
A mildly compressive dressing is placed on the lower face and neck. No compression is used on the scalp and periorbital area.
