Reversing Brow Lifts
Background: Undesirable brow shape and position may occur after brow lift surgery. Problems can include over elevation of the brows, separation of the brows, and creation of an apex medial slant brow shape.
Objective:We report on a procedure to restore or improve presurgical brow shape and position.
Methods: Brow lift reversal surgery was performed with open approaches. Anterior and posterior scalp flaps were developed in a subperiosteal plane. The lowered medial brow was sutured to the frontal bone with an anchor system. The repositioned anterior hairline was secured in a similar manner. The scalp defect that results was closed by advancing the posterior scalp flap. Galeal scoring was sometimes necessary to increase the length of the posterior flap.
Results: Twenty-two women (average age 45 years; range 32 to 62 years) presented for correction of their brow position and shape after brow lift surgery. All brows were lowered, and the brow apex was shifted laterally. The medial brow was lowered 3 to 10 mm (average, 6 mm) relative to the intercanthal line. The anterior hairline was lowered 5 to IS mm (average 12 mm). The repositioning has remained stable over 6 months to 3 years’ follow-up. No revisionary surgery has been requested. Two patients bad areas of alopecia develop in the posterior scalp flap.
Conclusions: The surgically lifted brow can be lowered and reshaped by advancing, repositioning, and fixing the frontal scalp to the skull. (Aesthetic SurgJ 2007;27:367-375.)
Young, attractive women have low brows. In their analysis of eyebrow shape and position of attractive models from popular fashion magazines, Gunter and Antrobus1 found that, although there was individual variation, the brows usually started low medically and often were flat as they ascended slightly to the midpupil (Figure 1). Troilius2 noted that surgeons are creating too many unnaturally high brows as compared with the features of today’s young models. It is not uncommon for brow lift operations (both open and closed) to raise the brow to positions much higher and to configurations much different than those seen in youth. This elevation makes the patient look not only different but also older, by hollowing the upper lids and raising the hairline.
The aesthetic outcome of contemporary brow lift operations performed through both open and endoscopic techniques has been challenged by objective analyses that surveyed cosmetologists, plastic surgeons, and lay people. Freund and Nolan ’ tested the opinions of 11 cosmetic surgeons and 9 cosmetologists with computer graphics to isolate changes in brow shape or position as the only variables of appearance. They concluded that the medial brow should be located at or below the supraorbital rim, not above it, and that the brow should he shaped with its highest point located lateral to the pupil (“apex lateral slantâ€). When they evaluated 16 frequently referenced articles on brow lifts, they concluded that standard open and endoscopic brow lift operations frequently result in unsatisfactory eyebrow height and shape judged by these criteria. The postsurgical brows were frequently placed too high, with their shape changed from one with an apex lateral slant to a less desirable flat or apex medial slant.
Swift et al4 evaluated brow position 1 year after endoscopic brow lift surgery in 20 patients. They found that the brow elevation was long lasting but that there was an over-elevation medially. They concluded that this result may not be the most aesthetically pleasing eyebrow shape and position. When Schreiber et al5 surveyed 100 randomly selected lay people regarding the most pleasing shape and position of the brow, they found the general public’s idea of an aesthetically pleasing eyebrow to be different from typical brow lift results. The audience at the 85th Annual Meeting of the American Association of Plastic Surgeons was polled on the appearance of a patient’s pictures taken before and after endoscopic brow and midface lift. These images were taken from an article published in the plastic surgery literature. Fully 86% of the audience preferred the appearance of the patient before her surgery.6
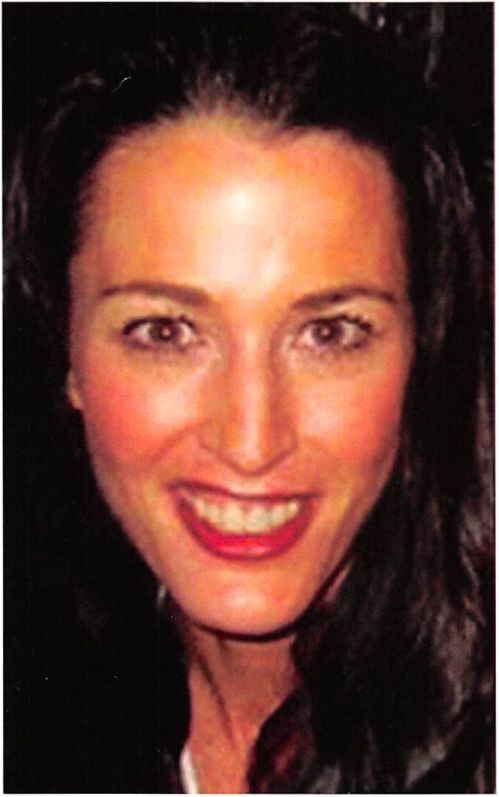
Figure 1. A young model who demonstrates the low brow position typically seen in popular fashion magazines.
The disparity between aesthetic ideals and surgical outcome has also been a concern to many patients who have undergone brow lift surgery. Although the surgical lowering of high hairlines has been addressed previously,/,s lowering and reshaping brows that have been elevated by surgery has not. Guyuron9 wrote that the most undesirable outcome of endoscopic brow lifting is excessive elevation of the brows and that its correction was difficult.
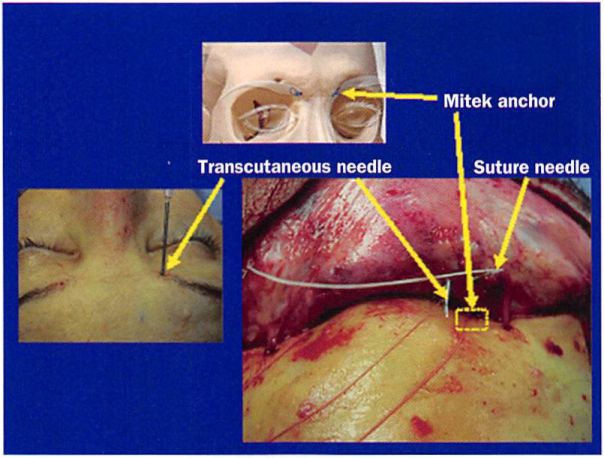
This article presents our method for lowering brows that have been surgically lifted, creating an appearance displeasing to the patient. Using an open approach, the anterior scalp flap was re-elevated in a subperiosteal plane down to the supraorbital rim. Suture/anchor systems (De Puy Mitek, Norwood, MA) placed in the frontal bone at a predetermined distance above the medial canthus were used to provide stable fixation for the repositioned medial brow. The posterior scalp flap was advanced anteriorly to compensate for the requisite downward movement of the anterior scalp flap. The anterior scalp flap was also sutured to a bone anchor positioned at the reestablished hairline to prevent any posterior migration. This procedure has been effective in 22 patients.
Patient population
Twenty-two women presented for correction of their brow position after previous brow lift surgery. The average age was 45 years (range 32 to 62 years). The average interval between their brow lift surgery and presentation for corrective surgery was 3 years (range 1 to 10 years). Most patients (n = 15) had had surgery performed endoscopically.
All patients presented with the chief complaint that their brows were positioned too high after brow lift surgery. Eighty percent of these patients also believed that their medial brows had become spread apart and were particularly high, giving their brows an undesired shape. Their desire was to look the way they did before brow lift surgery. Before surgery, a desired brow height and shape was agreed on with each patient.
Operative technique
Brow lift reversal surgery was performed with open approaches. Anterior and posterior scalp flaps were developed in a subperiosteal plane. The lowered medial brow was secured to the frontal bone by means of a Mitek anchor. The repositioned anterior hairline was secured in a similar manner. The scalp defect that results was closed by advancing the posterior scalp flap (Figure 2).
Incisions
Bicoronal or hairline incisions were used. Patients who had their brow lift surgery performed through a bicoronal approach had their brow lowering surgery performed using this same access. An incision placed in the anterior hairline created a narrow bipedicle flap between the hairline incision and coronal scar.
All but three of the patients who had their surgery done endoscopically had their brows lowered with bicoronal incision access. The remaining three patients desired their hairlines brought to a position lower than their pre-brow lift position. A hairline incision was used in these patients.
Brow repositioning
Before flap elevation, the skull was scored with a drill directly beneath the scalp incision. The position of the anterior hairline was similarly registered.
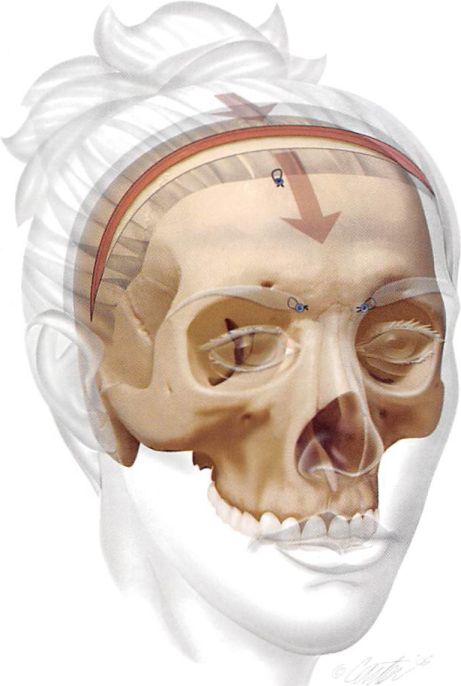
Figure 2. Overview of brow repositioning procedure. At the site of tire coronal incision and the present hairline, the skull is marked with a drill for later reference. Mitek anchors are placed at predetermined places in the glabellar area relative to the medial canthi. Their sutures purchase the posterior scalp directly beneath the medial aspect of the brow. A Mitek anchor is also used to reposition the anterior hairline. Tire scalp defect resulting from advancement of the anterior flap is closed by mobilizing and advancing the posterior scalp flap. It may he necessary to score the galea of the posterior flap to increase its surface area and therefore allow adequate advancement.
These registration marks would later serve as reference points during scalp and hairline repositioning. The anterior scalp flap was freed by subperiosteal dissection well onto the nasal root medially and the supraorbital rims laterally.
The brow was repositioned relative to the medial can- thus with a Mitek anchoring system. The Mitek anchor was originally developed for use in orthopedic surgery to secure muscle, ligament, and tendon to bone. The anchor is a titanium alloy cylinder with wings in its midbody and, in its posterior aspect, an eyelet that allows threading of sutures.
An inserter device was used to place the anchor into a hole prepared with a standard Mitek drill bit, which has a stop to prevent deep penetration. The wings were pressed against the body of the anchor as they were passed through more dense cortical bone and were reopened when they entered the frontal sinus (brow repositioning) or diploe (hairline repositioning). This locked the anchor into place.
A Mitek anchor was secured in the frontal bone at the desired distance (usually 15 to I 8 mm) directly above each medial canthus. The inevitable penetration of the frontal sinus by this anchor was of no clinical significance.
Because the nasofrontal suture is easily palpable through the skin and clearly visible when the scalp flap is reflected, it was a useful reference when positioning the anchor. A 19-gauge needle was positioned at the most inferomedial aspect of the brow and passed through the scalp flap. This marked the area for Mitek anchor suture purchase (Figure 3). The sutures were tied, thus securing the posterior aspect of the flap and hence, the medial aspect of the brow on its anterior surface, to its desired position.
Reversing Brow Lifts
Figure 3. Detail of medial brow fixation. Diagram shows position of anchor directly above the medial cant hits and approximately at the level of the nasofrontal suture (14 to IS mm above the medial canthus). Intraoperative view shows position of anchor (in box outline), transcutaneous needle used to determine position of medial brow relative to posterior surface of flap, and needle of suture attached to anchor.
Depending on the plan, this would reposition the medial brow 3 to 8 mm inferiorly and 1 to 3 mm medially.
The midbrow and lateral brow was repositioned as determined by patient preference. Most often, an “apex lateral slant†appearance was created through manipulation of the lateral aspect of the scalp flap. This position is secured by suturing the galea beneath the hair-bearing skin over the tail of the brow to the deep temporal fascia.
With the incision and hairline registration marks placed earlier used as references, the anterior hairline was repositioned. This position was also secured with Mitek anchor scalp fixation to the skull positioned just off the midline to avoid any possible sagittal sinus penetration.
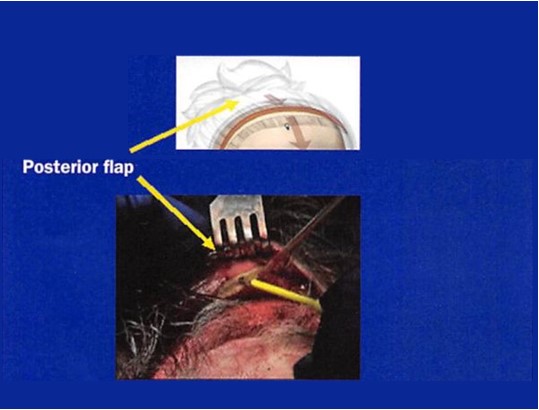
Posterior scalp flap advancement
Brow and hairline lowering inevitably leaves a gap between the anterior and posterior scalp flaps. In patients who have had their brow lift surgery performed endoscopically, no scalp was removed and the gap reflects tissue repositioned posteriorly. Sufficient tissue could be recruited from the posterior flap by widely undermining it back to the occiput and advancing it anteriorly.
In patients who have had their brow lift surgery per-formed through an open approach, the gap reflects scalp that has been excised. Filling this defect required serial scoring of the galea to expand the scalp surface area, as well as wide undermining and posterior scalp advancement (Figure 4). It was sometimes necessary to elevate the posterior scalp flap beyond the occiput to obtain sufficient posterior scalp flap length and forward movement. ,8
Results
In this series of 22 women whose brows were repositioned after previous brow lift surgery, the medial brow was lowered 3 to 10 mm (average 5 mm) relative to the intercanthal line. The anterior hairline was lowered 5 to 18 mm (average 10 mm).
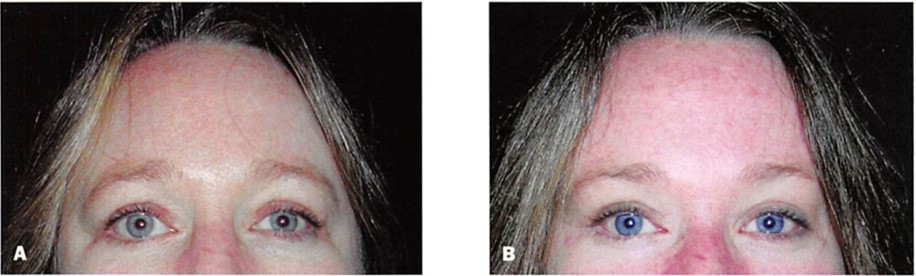
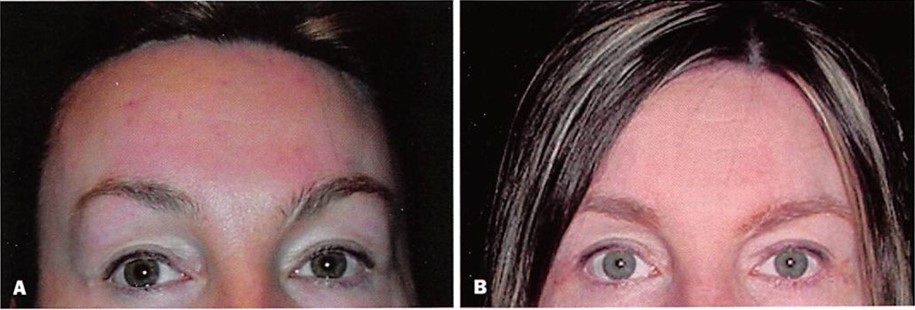
The repositioning has remained clinically stable during follow-up ranging from 6 months to 3 years (average, 18 months). No revisional surgery to reposition the brow or hairline has been requested. Two patients developed areas of alopecia in the posterior scalp flap after galeal scoring. One of these patients had a 10 X 25 mm area of alopecia excised and closed. Clinical examples of patients who have had this surgery are shown in Figures 5 through 8.
Discussion
Brow lifts are performed with the rationale that they are rejuvenating, because aging and gravity could only bring the brows down to a lower level However, objec-tive, subjective, and anecdotal observations show that the brow position and shape after many brow lifting procedures may be neither youthful looking nor attractive.1’6
Figure 4. Detail of posterior scalp flap advancement. Intraoperative view it shows scoring of posterior scalp flap galea to allow flap advancement.
This paradox can be explained by a lack of normative data, unclear aesthetic objectives, and the typical criteria for success. Because there is a paucity of normative data regarding brow height and position in youth and age, formulation of an aesthetic objective regarding rejuvenation of the brow remains unclear. Most brow lift articles base their efficacy on the long-term elevation of the brows. This implies that higher brows are more attractive brows, which is often not the case. Finally, contemporary brow lifting procedures have evolved into techniques that address not only brow height, but also transverse and vertical forehead wrinkles. The manipulations of the forehead musculature that ameliorate these wrinkles tend to impact negatively on brow shape and position.
There is only one report that examines brow position in women and how it changes with age; van den Bosch et al111 performed a cross-sectional cohort study examining the effect of age and sex on the topographic anatomy of periorbital structures, including the brows. In their study, 320 control subjects aged between 10 and 89 years were grouped as 10-year cohorts, and various surface measurements were made. When the distance between the upper lid margin and the lower border of the brow at midpupil was measured, the authors found that aging raised eyebrows in men and women. The serial photographs of the woman shown in Figure 9 support these findings.
There are two mechanisms that might explain why brows elevate with age. One explanation is that some women chronically elevate their brows to clear their visual field from redundant upper lid skin. Support for this mechanism comes from the observation that the brow is known to descend after upper lid blepharoplasty, presumably because there is no stimulus to clear the vision by raising the brow.11 Another explanation for brow elevation with aging is that aging results in levator disinsertion with resultant upper lid ptosis, since the study by van den Bosch et al10 also showed that aging caused an elevation in the upper lid skin crease. Ramirez12 also noted and attributed the elevated brow position seen in some patients with aging to clinical or subclinical weakness of the levator system. He coined the term “spastic frontalis syndrome†to describe this finding. The fact that patients with unilateral ptosis chronically raise the brow on the affected side also gives support for this theory.
The other available data regarding brow position in women at different ages use different landmarks and techniques for measurement, precluding direct comparison. In a study group consisting of 40 North American white women ages 19 to 25, Farkas et al13 found the average distance measured from midpupil obliquely to the upper border of the brow, with the subject in the recumbent position, was 26 mm. When the projection of the supraorbital rim is taken into account, the average distance was 23 mm (measurement of the patient in the correct position would give a smaller number).
Figure 5. A, Preoperative view of the 33-year-old woman shown in Figure I. B, Postoperative view I year after endoscopic brow and mid/ace lift and upper and lower lid blepharoplasty. C, Postoperative view 1 year after brow reversal surgery and subperiosteal midface lift.
Figure 6. A, Preoperative view of a 43-year old woman who had undergone endoscopic brow and mid face lift 2 years previously. She was displeased with her brow and hairline positions, as well as her lower lid asymmetry. B, Postoperative view I year after brow reversal surgery. A coronal approach was used to lower the medial brow 3 mm and the hairline 7 mm. A subperiosteal mid face lift was also performed.
McKinney et al14 and Zukowski1’1 measured the distance from the midpupil to the upper border of the high point of the eyebrow arch in 50 normal and healthy female volunteers with aesthetically pleasing facial appearance, ages 14 to 32. They found the average distance to be 25 mm.
The only objective data regarding brow height in older women come from the preoperative measurements of brow height in studies comparing the long-term efficacy of various brow lifting procedures. Swift et al4 found the preoperative average height in 20 patients, average age 54, to be 23.7 ± 3.4 mm from the lateral limbus to the upper border of the brow and 22.3 ± 4.0 mm from the lateral canthus to the upper border of brow. By combining two studies by Troilius,2’11 who measured brow height relative to fixed anatomic points before and after various brow lift procedures in 120 women, the average preoperative distance between midpupil and the top of the brow was 23 mm.
Analysis of these studies reveals several interesting facts regarding brow height and brow lift. It shows that, with aging, there is little change in the height of the brow at the vertical plane of the midpupil hut that there is descent laterally. Knize’s cadaver studies16 provide an anatomic explanation for this finding and commonly held clinical observation. These data also suggest that, save for the lateral brow, there is little difference in brow height between young women and those undergoing brow lifts. Successful brow lifts routinely raise brows to levels higher than those seen in youth.4,11
There are no objective data documenting a normal brow shape. However, the beauty industry and plastic surgery literature have been consistent as to what they perceive as an ideal shape. This has long been described as Westmore’s model, as referenced by Ellenbogen.17 Cosmetology texts describe the ideal shape of women’s brows as they relate to other facial features as the following: the eyebrow begins medially at a vertical line
Figure 7. A, Preoperative view of a 52-year-old woman who had undergone endoscopic brow lift 9 years earlier. Multiple procedures, including fullthickness skin grafts, had been performed in attempts to correct tower lid malposition after blepharoplasty. The patient desired her hairline to be lower than it was before brow lift surgery. B, Postoperative view 2 years after brow reversal surgery. Through a hairline incision, the medial brows were lowered 5 mm and the frontal hairline 15 mm. A subperiosteal midface lift, infraorbital rim augmentation, and lateral canthopexy were also performed.
Figure 8. A, Preoperative view of a 40-year-old woman who had undergone modified hairline hrotv lift I year earlier. B, Postoperative view 1 year after brow reversal surgery. Through the hairline incision, the medial brows were lowered 5 mm, and the frontal hairline was lowered 12 mm.
drawn perpendicularly through the ala of the nose; the lateral brow terminates at an oblique line drawn through the ala of the nose and the lateral canthus; the medial and lateral ends lie at approximately the same horizontal level; the apex of the brow lies on a vertical line directly above the lateral limbus.18 The shape of the eyebrow is described by the position of its apex relative to the midpupil. The preferred position is one with an apex lateral slant.3 In their analysis of eyebrow shape and position of attractive models from popular fashion magazines, Gunter and Antrobus1 found that, although there was individual variation, the brows usually started low medially and often were flat as they ascended slightly to the midpupil (Figure 1). As previously discussed,2 ‘’ contemporary open and endoscopic procedures rarely produce a brow with this shape. Rather, the tendency for today’s postoperative brows is to have predominant medial elevation or an apex medial slant.
Freund and Nolan3 pointed out that most brow lift articles avoid stating aesthetic objectives. These articles focus on surgical techniques and illustrate results. Success is not judged on improved appearance but rather on the amount and stability of lifting. For example, Troilius11 compared the long-term results of bicoronal
Figure 9. A-E, Serial photographs of a woman taken at ages 13, 25, 31, 38, and SO years, respectively. Note that the brows are elevating with time.
subgaleal brow lifts with endoscopic subperiosteal brow lifts. He found that at 1 year after subgaleal lifts, the vertical height of the brow returned to the preoperative level, except for its lateral aspect. He stated that this lateral elevation made the patient look better than they did before surgery, even though the overall height of the brow was the same or even lower than it was before surgery. He found that the elevation after endoscopic subperiosteal lifting was long lived and, on the basis of this criterion, as well as the fact that it avoided issues related to the open approach, deemed it superior to the open subgaleal approach.
Although designated a “brow lift†operation, contemporary brow lift procedures have three basic goals: elevation of the brows, reduction of transverse forehead lines, and attenuation of vertical glabellar furrows.19 Creating an open appearance of the eyes and making patients look less tired and angry are also frequently mentioned indications for this procedure.20 Improvement of brow aesthetics is not the sole purpose of this procedure and, as noted by Matarasso and Terino,21 is often a lesser consideration. Weakening or removal of the corrugator and procerus muscles allows the medial brows to elevate and separate. Daniel and Tirkanits22 documented that the medial brow was elevated 2 mm after corrugator-procerus muscle resection as a result of the unopposed frontalis muscle. Behmand and Guyuron23 showed that there was consistent elevation and increased distance between the medial brows after corrugator and procerus resection. Rather than apex lateral slant, the shape becomes one of apex medial slant, with the medial brow starting far lateral to the nasal ala. This shape is demonstrated in the preoperative views in this article.
Conclusion
Elevated brows are not necessarily attractive or youthful-appearing brows and, in many instances, brow lift surgery can make patients look both different and older. The surgically lifted brow can be lowered and reshaped by advancing, repositioning, and fixing the frontal scalp to the skull. This procedure offers the opportunity to restore or improve presurgical brow shape and position. â–
The authors have no financial interest in and receive no compensation from manufacturers of products mentioned in this article.
References
1. Gunter JP. Antrobus SD. Aesthetic analysis of the eyebrows. Plast Reconstr Surg 1997;99:1808-1816.
2. Troilius C. Subperiosteal browlifts without fixation. Plast Reconstr Surg 2004;114:1595-1603.
3. Freund RM, Nolan WB. Correlation between brow lift outcomes and aesthetics ideals for eyebrow height and shape in females. Plast Reconstr Surg 1996;97:1343-1348.
4. Swift RW. Nolan WB, Aston SJ. Basner AL. Endoscopic brow lift: objective results after 1 year. Aesthetic Surg J 1999:19:287-292.
5. Schreiber JE, Singh NK. Klatsky SA. Beauty lies in the eyebrow of the beholder: a public survey of eyebrow aesthetics. Aesthetic Surg J 2005:25:348-352.
6. Audience response system data from Periorbital Aesthetic Surgery panel presented at the 85th Annual Meeting of the American Association of Plastic Surgeons, Hilton Head. South Carolina, May 2006.
7. Guyuron B, Behmand RA, Green R. Shortening of the long forehead. Plast Reconstr Surg 1990;103:218-223.
8. Marten T. Hairline lowering during foreheadplasty. Plast Reconstr Surg 1999;103:224-236.
9. Guyuron B. Endoscopic forehead rejuvenation: I—limitations, flaws, and rewards. Plast Reconstr Surg 2006:117:1121-1133.
10. van den Bosch W. Leenders I, Mukler P. Topographic anatomy of the eyelids, and the effects of sex and age. Br J Ophthamol 1999;83:348-352.
11. Troilius C. A comparison between subgaleal and subperiosteal brow lifts. Plast Reconstr Surg 1999:104:1079-1090.
12. Ramirez OM. Discussion of Troilius C. Subperiosteal browlifts without fixation. Plast Reconstr Surg 2004;114:1595-1603.
13. Farkas LG, Hreczko TA. Katie MJ. Craniofacial norms in North American Caucasians from birth (one year) to adulthood. Appendix A. In Farkas L.G. ed. Anthropometry of the Head and Face. 2nd ed. New York: Raven Press; 1994. p. 241-333.
14. McKinney P. Mossie RD. Zukowski ML. Criteria for the forehead lift. Aesthetic Plast Surg 1991:15:141-147.
15. Zukowski ML. Clinical evaluation of the blepharoplasty patient with brow ptosis. Aesthetic Surg J 1998:18:51-52.
16. Knize DM. An anatomically based study of the mechanism of eyebrow ptosis. Plast Reconstr Surg 1996:97:1321-1333.
17. Ellenbogen R. Transcoronal eyebrow lift with concomitant upper ble- pharoplasty. Plast Reconstr Surg 1983:71:490-497.
18. Maron M. Makeover miracles. 1st ed. New York: Crown Publishers: 1994. p. 50-53.
19. Elkwood A, Matarasso A. Rankin M. Elkowitz M, Godek CP. National plastic surgery survey: brow lifting techniques and complications. Plast Reconstr Surg 2001:108:2143-2152.
20. De Cordier BC, de la Torre Jl, Al-Hakeem MS. Rosenberg LZ. Gardner PM. Costa-Ferreira A, et al. Endoscopic forehead lift: review of technique, cases, and complications. Plast Reconstr Surg 2002:110:1558-1570.
21. Matarasso A, Terino EO. Forehead-brow rhytidoplasty: reassessing the goals. Plast Reconstr Surg 1994:93:1378-1389.
22. Daniel RK, Tirkanits B. Endoscopic forehead lift: an operative technique. Plast Reconst Surg 1996;98:1148-1157.
23. Behmand RA, Guyuron B. Endoscopic forehead rejuvenation: II. Long term results. Plast Reconstr Surg 2006:117:1137-1143.