Mandibular Augmentation
Porous polyethylene implants are available that are designed to augment the mandibular ramus and body. They can be used to increase the bigonial distance in patients with normal mandibular anatomy who desire an increase in lower facial width. When used in combination with extended chin implants, they can camouflage the skeletal contour inadequacies associated with class II mandibular deficiency. The implants are placed through intraoral incisions and fixed with titanium screws. In a clinical experience with 11 patients over 6 years, this technique has proven to be safe and effective. (Plasl. Rcconstr. Surg. 106: 697, 2000.)
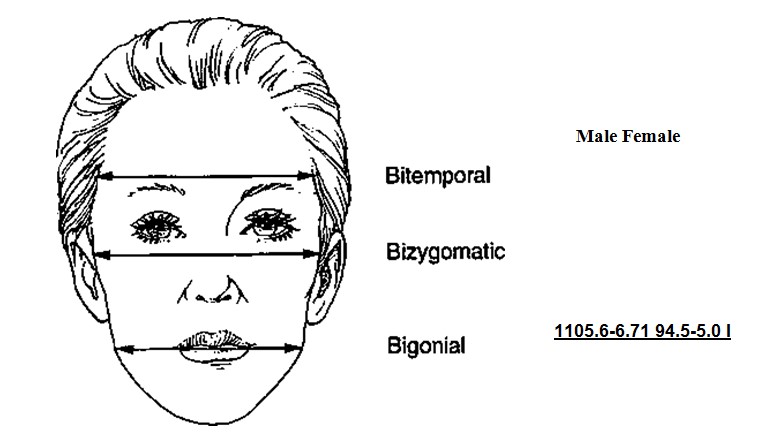
Alloplastic augmentation of the mandibular ramus and body can have a dramatic impact on the appearance of the lower third of the face. Two patient populations have had their aesthetic concerns satisfied with mandibular augmentation procedures. One group has mandibular dimensions that relate to the upper and middle thirds of the face within the normal range (Fig. I).1 These patients perceive a wider lower face as an enhancement to their appearance. Patients in this treatment group often present with a desire to emulate the appearance of models, actors, and actresses who have a defined, angular lower face. This patient group benefits from implants designed to augment the ramus and posterior body of the mandible and, in so doing, increase the bigonial distance.
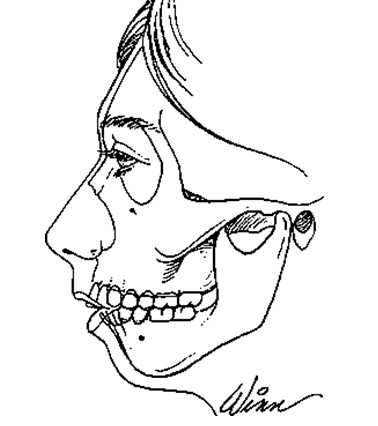
The other major group of patients who benefit from augmentation of the mandibular ramus and body includes those patients with skeletal mandibular deficiency. It has been estimated that approximately 5 percent of the total United States population has skeletal mandibular deficiency resulting in a class II occlusal problem (Fig. 2).2 The majority’ of these patients (approximately 80 percent) can have their dental relationships normalized through orthodontic tooth movement. The remaining 20 percent, or 1 percent of the total population, have mandibular deficiency that is so severe that surgical mandibular advancement would be needed to correct it.2 Those patients who have their malocclusion treated with orthodontics alone are left with mandibular skeletal deficiencies, which may be deforming. The skeletal anatomy associated with mandibular deficiency, which can be camouflaged with implants designed to augment the ramus and body of the mandible, includes the obtuse mandibular angle with steep mandibular plane, as well as the decreased vertical and transverse ramus dimensions. The addition of an extended chin implant will camouflage the poorly projecting chin.
The concepts presented in this article are developed from those of Terino,3-4 Whitaker/’ and Aiche.6 Alloplastic augmentation of the mandible, until recently, was confined to increasing the projection of the mentum with small implants.7,8 Terino8-4 developed extended chin implants that augmented not only the central mentum but also the mandibular body. This type of implant widened the anterior jaw line in addition to increasing the projection of the chin. Whitaker5 described his experience with a posterior implant designed specifically to increase lower facial width. Aiche6 described an implant for the mandibular angle that augmented this area in three dimensions. Taylor and Teenier9 presented their use of a similarly shaped mandibular angle implant. Whereas the indications for mandibular augmentation were primarily aesthetic and the surgery was performed through intraoral incisions in the above series, Semergidis et al.10 recently presented their experience with the use of porous polyethylene implants to correct an obtuse gonial angle in posttraumatic and postreconstructive deformities through external incisions.
Fig. 1. Normal values in millimeters for upper, middle, and lower facial width in North American Caucasian adult men (ages 19 to 25) (n = 109) and young adult women (n = 199).1 Bitemporal distance is measured from frontotemporal, which is the point on each side of the forehead, laterally from the elevation of the linea temporalis. Bizygomatic distance is measured from zygion to zygion, which is the most lateral point of each zygomatic arch. The bigonial distance is measured from gonion to gonion, which is the most lateral point of the mandibular angle close to the bony gonion.
This article describes the use of alloplastic implants to augment skeletal dimensions in patients with both normal-sized and underdeveloped mandibles. Implant design, implantation technique, and experience with their use are presented. This article shows that favorable aesthetic changes can be made in the lower third of the face with an outpatient procedure associated with a low rate of morbidity.
THE IMPLANTS
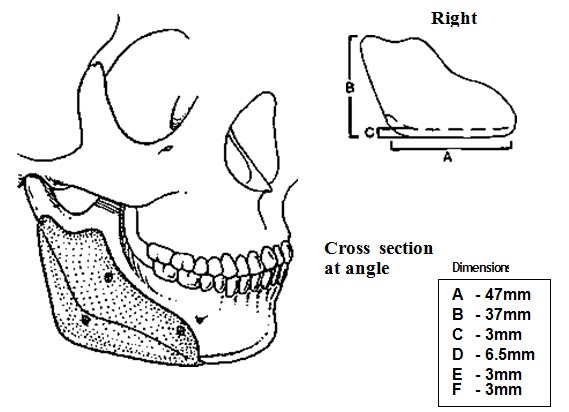
Two basic designs of ramus and body implants have been used, alone or in combination with extended chin implants, depending on the patient’s aesthetic needs. To date, all ramus and body implants have been made of porous polyethylene (Porex Surgical, College Park, Ga.), whereas the chin implants have been made of porous polyethylene or silicone and produced by various manufacturers. One implant is used primarily to increase lower facial width by augmenting the mandibular ramus and posterior body. Its configuration and dimensions are presented in Figure 3.
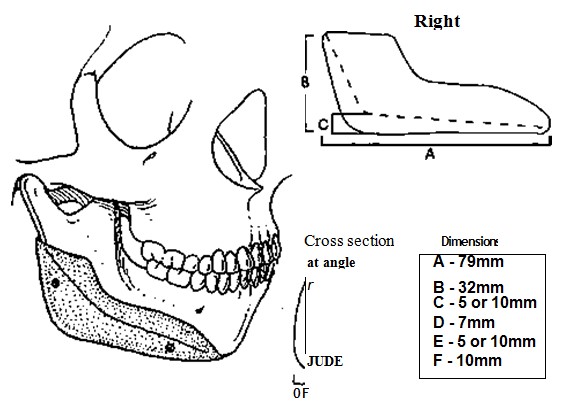
The other implant is used to augment the congenitally deficient mandible. Its dimensions are presented in Figure 4. It differs from the other implant in several ways. In addition to augmenting the ramus and posterior body, its greater length (A) allows it to augment the anterior body of the mandible. It, therefore, increases not only posterior but also anterior mandibular width. Its tapering projection beyond the inferior edge of the mandible (C and E) allows it to change the inclination of the plane of the mandibular border. Because it also projects beyond the posterior border, in addition to extending beyond its inferior edge of the ramus, it can lessen the obliquity of the mandibular angle. All dimensions of the implant may be trimmed to meet the aesthetic needs of the patient.
Extended chin implants are routinely used in patients treated for mandibular deficiency. They may be trimmed and positioned to meet the aesthetic needs of the patient (Fig. 5).
PREOPERATIVE PLANNING
Physical examination is the most important element in preoperative assessment and planning. Reviewing life-size posteroanterior and lateral photographs with the patient can be helpful when discussing aesthetic concerns and goals. To allow the patient to understand the scale and scope of augmentation, it is useful to have sample implants available to demonstrate on a model skull and to apply these implants to the relative area of the patient’s face.
Posteroanterior and lateral cephalograms provide data that help the surgeon determine how the dimension of the implant might be altered to best suit the patient. In general, however, the size and position of the implant are largely aesthetic judgments. An approximately 1:1 ratio of augmentation to resultant projection is anticipated.
OPERATIVE TECHNIQUE
This procedure is done under general anesthesia using nasotracheal intubation. The face and oral cavity are prepared with an iodine solution after placement of a throat pack. The operative site is infiltrated with Vkoo.ooo epinephrine solution to provide hemostasis.
A generous intraoral mucosal incision is made to expose the ramus and body of the mandible. It is made at least 1 cm above the sulcus on its labial side (Fig. 6). The anterior ramus and body of the mandible are freed from their soft tissues. If the mental area is also being augmented, a submental incision is made for access and exposure of the anterior mandible. The inferior alveolar nerve is visualized as it exits its foramen to avoid its injury. It is important to free both the inferior and posterior borders of the mandible of soft-tissue attachments to allow implant placement.
As determined by preoperative assessment, the implant is trimmed with a scalpel before its placement on the mandible.
Fig. 2. Soft-tissue contour and skeletal configuration of patient with mandibular deficiency with class II malocclusion.Â
Fig. 3. Configuration and dimensions of mandibular ramus and posterior body implant used to increase lower facial width. Screw fixation guarantees position and assures application of implant to skeleton.
Fig. 4. Configuration and dimension of mandibular ramus and mandibular body implant used to augment the deficient mandible. Because it extends beyond the posterior border of the ramus and inferior edge of the ramus and body, it closes the mandibular angle and lessens the plane of the mandibular border. Screw fixadon guarantees posidon and ensures applicadon of implant to skeleton
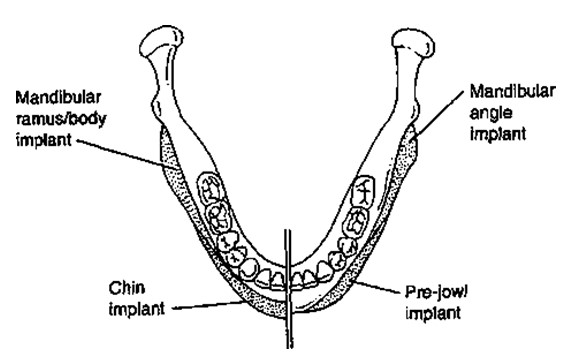
Fig. 5. Axial view of mandible showing two possible implant combinations. On the right is a simulation of the implant illustrated in Figure 3 used in combinadon with a prejowl implant.17 On the leftside, an implant similar to that used in Figure 4 is combined with an extended chin implant. This combination may be used for patients with class II mandibular deficiency.
Fig. 6. Intraoral mucosal incision is made along ramus and posterior body of mandible. It is made approximately 1 cm above the sulcus on its labial side.
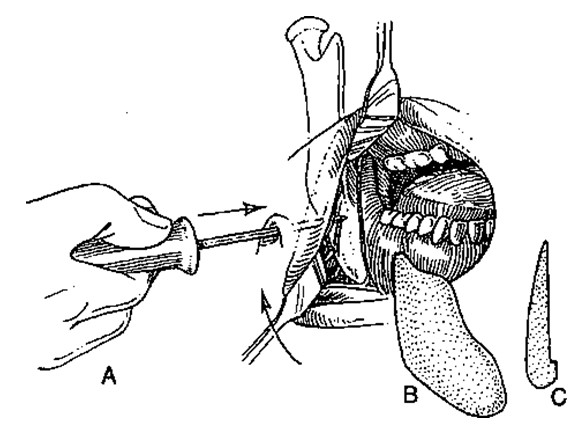
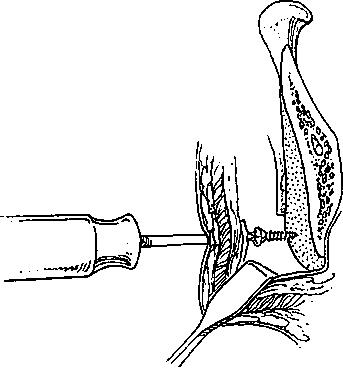
To ensure the desired placement of the implant and its application to the surface of the mandible, the implant is fixed to the mandible with selfdrilling, titanium screws (Synthes, Paoli, Pa.). Stab wound incisions (2 to S mm) are made in the neck skin beneath the inferior border of the mandible. The screwdriver is then gently manipulated through the intervening soft tissues and into the operative field (Fig. 7). This allows strategic unicortical screw fixation of the implant to the mandible (Fig. 8). Usually two or three screws are used to obliterate any gaps between the mandible and the implant. Screws are placed to avoid the anticipated path of the inferior alveolar nerve before its exit from the mental foramen.
It is crucial to soften any transitions between the implant and the mandible, particularly where the implant extends beyond the anterior mandibular border’s inferior edge. Any step- offs between the implant and the mandible in this area may be visible in thin patients. Screw fixation of the implants allows scalpel or mechanical burr final contouring with the implants in place.
Fig. 7. (Left) A stab wound incision is made in the neck skin to allow transcutaneous placement of a screwdriver for implant fixation. The screwdriver is gendy manipulated through the soft tissues between the skin and the operative field. (Center) Oblique view of implant. (Right) Lateral view of implant.
Fig. 8. Cross secuonal view shows unicortical screw fixation of implant to anterior surface of mandible
The incision is closed in two layers with absorbable sutures. Care is taken to evert the mucosal edges. Neither the operative field nor the implants have been treated with antibiotic solutions. An elastoplastic external dressing is used to help apply the soft tissues to the implant and avoid hematoma formation.
Patients are administered broad spectrum antibiotics (cephalosporins) intravenously immediately before the procedure. Oral antibiotics are administered for 5 days postoperatively.
A liquid diet is prescribed for the first 3 days postoperatively and a soft diet for the next 5 days. Frequent mouth washes are advised as well as very careful tooth brushing.
CLINICAL EXPERIENCE
Since 1994, 11 patients have undergone alloplastic augmentation of the mandibular ramus and body with porous polyethylene implants. There have been six women and five men. The average age has been 30 years with a range of 21 to 52 years. Three patients had normal skeletal relationships but underwent augmentation to increase facial width. Four patients had had orthodontic correction of class II dental malocclusion and desired camouflage of their mandibular deficiency. Three patients had posttraumatic asymmetry, and the third patient had asymmetry owing to hemifacial microsomia. Follow-up has ranged from 3 months to 4 years with an average of 2 years. There have been no infections and no implant exposures. There have been no permanent motor or sensory deficits. One female patient required reoperation at 1 week to correct asymmetry and poor transition between the mandibular border and the most anterior aspect of
the implant. With the exception of this patient, all patients have been satisfied with their ap
pearance after their initial surgery. Representative patient examples are presented in Figures 9 through 12.
DISCUSSION
Mandibular augmentation with porous polyethylene implants as described in this article has provided predictable aesthetic results with
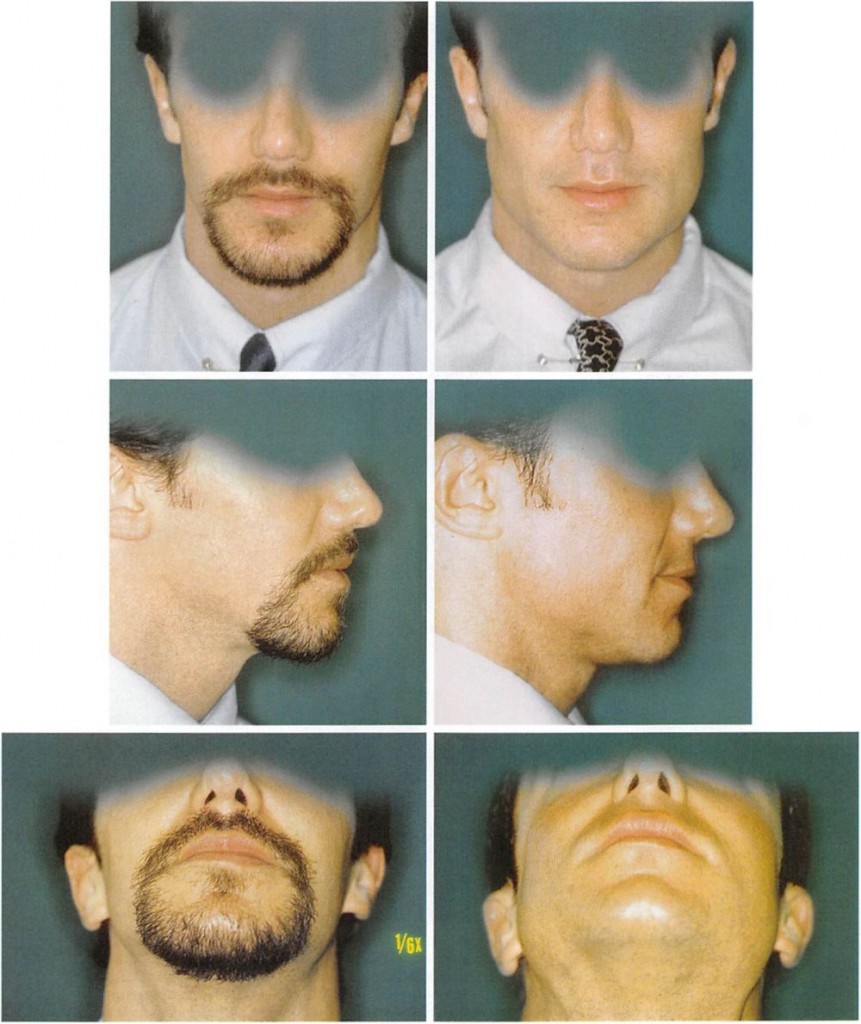
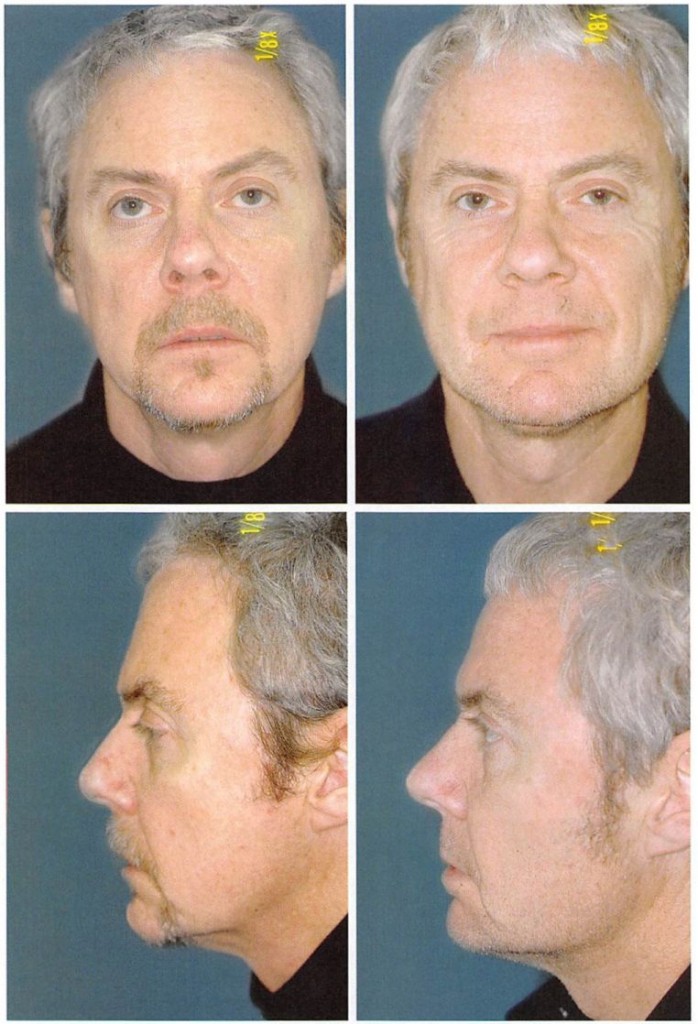
Fig. 9. A 30-year-old male actor with normal facial dimensions and class I dental occlusion desired more “strength†to his jaw and requested chin augmentation. After evaluation, a mandibular ramus and posterior body augmentation with the implants described in Figure 3 was performed as well as a tertiary rhinoplasty. (Above, left) Preoperative and (above, right) 6-month postoperative frontal views. (Center, left) Preoperative and (center, right) 6-month postoperative lateral views. (Below, left) Preoperative and (below, right) 6-month postoperative worm’s eye views.
Fig. 10. A 52-year-old man with normal skeletal dimensions and class I dental occlusion desired increased definition of the mandible. He was satisfied with the projection of his chin. Mandibular ramus and body augmentation was accomplished with a mandibular implant (Fig. 3) and an extended silicone implant divided, contoured, and positioned to augment the anterior mandible or prejowl sulcus area as described by Mittleman.17 The configuration depicted on the right side of Figure 5 is similar to that employed in this patient. (Above, left) Preoperative and (above, right) 6-month postoperative frontal views, (Below, lejl) Preoperative and (below, right) 6-month postoperative lateral views.
minimal morbidity. Alternative methods of mandibular augmentation include the use of
osteotomies, autogenous onlay grafts, and other alloplastic materials. These other options for treatment as well as the rationale and nuances of the methods presented here are discussed. For patients who have normal facial skeletal relations but who desire an increase in their lower facial width, sagittal osteotomy of the ramus with bone grafts interpositioned between the cortices has been performed. This procedure has been reported as technically demantling, time consuming, and expensive.511 It is, therefore, rarely clone. Augmentation of the posterior mandible with autogenous bone grafts was abandoned because of the varying success due to the unpredictable resorption of autogenous onlay grafts.5,11
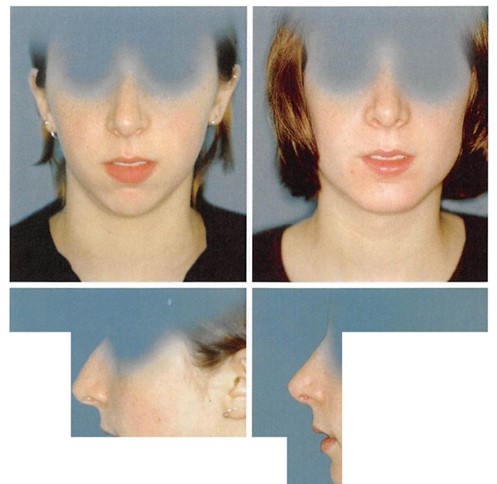
Fig. 12. A 26-year-old woman with normal facial skeletal relationships and class I dental occlusion desired increased angularity and definition of her malar midface and lower face. Malar augmentation was done with small design M malar implants (Porex Surgical, College Park, Ga.). The configuration depicted on the right side of Figure 5 is similar to that employed in this patient. Mandibular ramus, body, and prejowl augmentation was performed. {Above, left) Preoperative
The classic method of correcting class II dental malocclusion in patients with significant mandibular deficiency, in addition to preoperative and postoperative orthodontic treatment, involves sagittal split ramus osteotomy and sliding advancement genioplasty, with possible Le Fort I maxillary impaction. This combination of procedures is ideal in that it can provide a
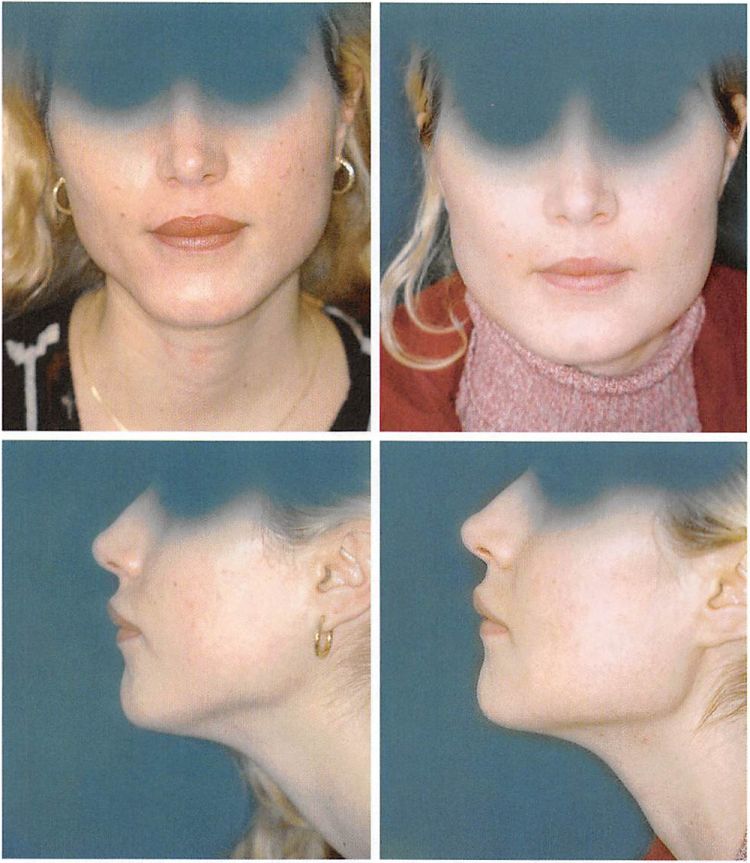
Fig. 11. A 21-year-old woman who had undergone orthodontic correction ol her class II malocclusion desired improved nasal and mandibular contour. Reduction rhinoplasty and mandibular augmentation with mandibular ramus and body implants (Fig. 4) were performed, together with an extended anatomic chin augmentation. The configuration employed on the left side in Figure 5 is similar to that cmpl right) 6-month postoperative frontal views. (postoperative lateral views. m this patient. {Above, left) Preoperative and {above, left) Preoperative and {below, right) 6-month
class I dental relationship while normalizing the skeletal contour. In patients with mandibular deficiency who have had their malocclusion corrected through orthodontics alone, mandibular osteotomy would disturb these dental relationships, requiring extensive perioperative orthodontic treatment. This type of treatment is both costly and time consuming. Alloplastic augmentation of the mandible can provide a visual effect similar to that of sagittal osteotomy with an outpatient surgical procedure that avoids any further dental manipulation.
The anthropometric measurements provided by Farkas1 (Fig. 1) help in understanding our visual interpretation of male and female patients with normal mandibular morphology and dimensions who undergo mandibular augmentation. These data show that all transverse facial dimensions are greater in men than in women and that the bigonial distance is the transverse facial dimension that has the greatest difference between the sexes. These data also reveal that the difference between bigonial width and bizygomatic width is greater in women (36 mm) than in men (34 mm). In other words, the lower one-third of women’s faces tends to be absolutely and relatively narrower than that of men. Hence, when normal male mandibles undergo augmentation, they may be perceived as stronger (Figs. 9 and 10). However, when normal female mandibles undergo augmentation, they may be perceived as masculinized (Fig. 12).
Other biomaterials used for mandibular augmentation include Proplast5 and silicone.6,9 In a series of 22 patients operated on over a 4-year period, Whitaker5 reported no infections and one intraoral exposure in a patient who had been previously irradiated for rhabdomyosarcoma. Using silicone implants, Aiche6 recorded two infections without indicating the number of cases performed. Semergidis et al. reported no infections in 18 patients who had undergone mandibular augmentation with porous polyethylene implants placed through external excisions.10 There have been no infections in our small series of patients, despite the fact that large implants were placed in a relatively dependent position through intraoral incisions. A low incidence of infection has been reported with the use of porous polyethylene for reconstruction of other areas of the facial skeleton.12-16
Several technical steps are believed to minimize morbidity and optimize the aesthetic outcome during this procedure. These involve precise incision placement and closure, avoidance of hematoma formation, and application of the implant to the mandible.
The intraoral incision is made at least 1 cm above the sulcus. This limits the likelihood of pooled saliva percolating through any defects in the wound closure and contaminating the operative site. A two-layer wound closure with care to evert the mucosal edges also reduces the likelihood of operative site contamination during the early postoperative period.
Screw fixation of the implant to the mandible has several benefits. It prevents any displacement of the implant. It also ensures application of the implant to the surface of the mandible. Because each mandible has a unique and varying surface topography, a non- conforming implant will leave gaps between the implant and the mandible. These gaps are problematic for two reasons. The space between the implant and the mandible is equivalent to an additional augmentation. This can lead to over augmentation and asymmetries. Gaps are also potential spaces for hematoma and seroma formation. Finally, screw fixation allows for final contouring with the implant in position. This final contouring is particularly important where the anterior aspect of the implant interfaces with the body of the mandible. Any step-off between the implant and the mandible will be palpable and possibly visible in thin-skinned patients. The 2- to 3-mm scars in neck skin resulting from the stab wound incisions for screw placement (Fig. 7, left) have not been noticeable in, or objected to by, any patient.
CONCLUSIONS
Augmentation of the ramus and body of the mandible with porous polyethylene implants fixed with screws has been effective in increasing the bigonial distance in patients with normal mandibular anatomy who desire an increase in lower facial width. When used in conjunction with extended chin implants, the mandibular body and ramus implants can effectively camouflage the deficient mandible.
Michael J. Yaremchuk, M.D.
Division of Plastic Surgery Massachusetts General Hospital, WACC-453 Boston, Mass. 02114 myaremchuk@partners. com
REFERENCES
1. Farkas, L. G., Hreczko, T. A., and Katie, M. J. Appendix A: Craniofacial Norms in North American Caucasians from Birth (One Year) to Young Adulthood. In L. G. Farkas (Ed.), Anthropometry of the Head and Face, 2nd Ed. New York: Raven Press, 1994.
2. Bell, W. H., Proffit, W. R., Chase, D. L., Wickwire, N. A., and Poulton, D. R. Mandibular  Deficiency. In W. H. Bell, W. R. Proffit, and R. P. White (Eds.), Surgical Correction of DentofacialDeformities, Vol. 1. Philadelphia: Saunders, 1980.
3. Terino, E. O. Alloplastic facial contouring: Surgery of the fourth plane. Aesthetic Plast. Surg. 16: 195, 1992.
4. Terino, E. O. Unique mandibular implants, including lateral and posterior angle implants. Facial Plast. Surg. Clin. North Am. 2: 311, 1994.
5. Whitaker, L. A. Aesthetic augmentation of the posterior mandible. Plast. Reconslr. Surg. 87: 268, 1991.
6. Aiche, A. E. Mandibular angle implants. Aesthetic Plast. Surg. 16: 3490, 1992.
7. Millard, D. R. Adjunct in augmentation mentoplasty and corrective rhinoplasty. Plast. Reconstr. Surg. 36:48, 1965.
8. Pitanguy, I. Augmentation mentoplasty. Plast. Reconstr.Surg. 42: 460, 1968.
9. Taylor, C. O., and Teenier, T. J. Evaluation and augmentation of the mandibular angle region. Facial Plast. Surg. Clin. North Am. 3: 329, 1994.
10. Semergidis, T. G., Migliore, S. A., and Sotereanos, G. C.
Alloplastic augmentation of the mandibular angle. J. Oral Maxillofac. Surg. 54: 1417, 1996.
11. Ousterhout, D. K. Mandibular angle augmentation and reduction. Clin. Plast. Surg. 18: 153, 1991.
12. Choi, J. C., Sims, C. D., Casanova, R., Shore, J. W., and Yaremchuk, M. J. Porous polyethylene implant for orbital wall reconstruction./ Craniomaxillofac. Trauma 1: 42, 1995.
13. Wellisz, T. Reconstruction of the burned external ear using a Medpor porous polyethylene pivoting helix framework. Plast. Reconstr. Surg. 91: 811, 1993.
14. Wellisz, T., and Dougherty, W. The role of alloplastic skeletal modification in the reconstruction of facial burns. Ann. Plast. Surg. 30: 531, 1993.
15. Rubin, J. P., and Yaremchuk, M.J. Complications and toxicides of implantable biomaterials used in facial reconstructive and aesthetic surgery: A comprehensive review of the literature. Plast. Reconstr. Surg. 100: 1336, 1997.
16. Yaremchuk, M.J., and Israeli, D. Paranasal implants for correction of midface concavity. Plast. Reconslr. Surg. 102: 1676, 1998.
17. Mittleman, H. The anatomy of the aging mandible and its importance to facelift surgery. Facial Plast. Surg. Clin. North Am. 2: 301, 1994.