Complex Orbital Fracture Repair Using Rigid Fixation of the Internal Orbital Skeleton
Large orbital fractures involving more than one orbital wall are frequently associated with enophthalmos and vertical globe dystopia. The authors repaired 22 orbits in 20 patients using the technique of rigid fixation of the internal orbital skeleton. Eleven orbits were reconstructed with titanium or vitallium implants that were custom-shaped to span the bony defect and fixed to the orbital rim. Seven orbits were reconstructed with bone grafts rigidly supported by a miniplate, and, in four cases, direct lag screw support of bone grafts was used. The intraoperative goal was to restore the native orbital anatomy and volume. Autologous calvarial bone grafts were used to supplement the repair to achieve the desired volumetric effect and to cover additional wall defects. A reoperation for additional orbital augmentation was needed in one enophthalmic and one anophthalmic orbit. There were no cases of overcorrection, migration, infection, or extraocular muscle entrapment. In complex orbital fractures, the technique of rigid internal orbital fixation appears to yield a stable and predictable result with the prevention of postoperative globe malposition. Ophthalmology 1992;99:553-559
Large orbital fractures, typically involving more than one wall, are frequently complicated by post-traumatic enophthalmos and vertical globe dystopia. The principle mechanism of post-traumatic enophthalmos is displacement of the orbital soft tissue into an enlarged bony orbit.12 For this reason, primary surgical repair should be directed at restoring the native bony orbital volume and contour, while repositing herniated orbital soft tissue.
Typically, these larger orbital fractures are repaired by first reducing and fixating the orbital rim with wires or miniplates.3 Next, the contour of the internal orbital walls are restored. Small defects can be spanned by onlay grafts of autogenous or alloplastic materials, thus restoring the desired orbital volume.
In cases of severe orbital trauma, with massive commination of the thin orbital bones, there is no stable platform on which to support a suitable implant. Historically, in such cases, support for orbital contents was achieved by temporarily obliterating the underlying maxillary antrum, thus providing a support for the orbital soft tissues and implants if needed.
Originally received: August 13, 1991. Revision accepted: October 31, 1991. 1 Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston. 2 Massachusetts General Hospital, Harvard Medical School, Boston. Reprint requests to Peter A. D. Rubin, MD, Eye Plastics and Orbit Center, Massachusetts Eye and Ear Infirmary, 50 Staniford St, Third Floor, Boston, MA 02114.
In other cases, where an implant was placed, it could only be positioned where the minimal intact bone would permit positioning. These techniques were complicated by enlarged orbital volume, implant migration, and recurrent/persistent globe malposition.
In an effort to overcome the limitations of previous techniques and to establish the desired rigid orbital volume, we have pursued the technique of rigid support of the internal orbital skeleton. Using malleable titanium plates that are fixed to the orbital rim, custom-shaped, and cantilevered to span the bony defects, stable mechanical support for the orbital soft tissues and establishment of the desired rigid orbital volume is achieved. Alternatively, bone grafts rigidly supported by a lag screw or fixated to a miniplate also serve to provide a stable platform for further orbital reconstruction. In our experience, we have found that this approach to these most challenging orbital fractures results in a stable, predictable operative outcome with the prevention of postoperative enophthalmos.
MATERIALS AND METHODS
Between August 1987 and February 1990, the authors repaired complex orbital fractures in 20 patients using rigid fixation of the internal orbit. All surgery was performed at Massachusetts General Hospital and Massachusetts Eye and Ear Infirmary. Two of these cases involved bilateral repair using this method, resulting in a total of 22 orbital fractures that were evaluated in this series. A minimum follow-up of 6 months was required for inclusion in this study. Fourteen of these fractures resulted from motor vehicle trauma, with assaults and other blunt trauma accounting for the rest. Most of these injuries were in the setting of panfacial and craniofacial trauma. Whenever possible, acute repair was performed; however, over-riding medical concerns and delayed referrals accounted for cases of late repair. Twelve patients underwent acute repair, and eight patients had delayed orbital reconstruction.
Surgery involved total subperiosteal exposure of the orbital rims combined with deep orbital exploration. A bicoronal and subciliary or inferior fornix approach was typically used to expose the orbit. Anatomic reduction of the orbital rim, zygomatic arch, maxillary buttresses, and frontal bone was achieved by rigid fixation with miniplates or less commonly with stainless steel wire before repair of the internal orbital skeleton. In this series, there was massive comminution of the orbital walls, such that an implant could not be securely placed in the desired position (Fig 1). Therefore, rigid internal orbital fixation methods were used.
One of three methods was used to obtain internal orbital fixation:
(1) custom orbital floor titanium plates (Synthes, Paoli, PA) or vitallium mesh (Howmedica, Rutherford, NJ) was fashioned to cover the defect and fixed to the orbital rim with self-tapping screws (Fig 2);
(2) autologous bone grafts were fixed to micro titanium plates (Howmedica) and anchored to the orbital rim; or
(3) lag screw fixation of autologous bone grafts. Additional bone grafts were placed on these implants as needed to achieve the desired volumetric effect and to cover additional orbital wall defects (Figs 3 and 4). Postoperative plain films or computed tomography scans were obtained in each case to confirm positioning of the orbital implants (Figs 4 and 5). 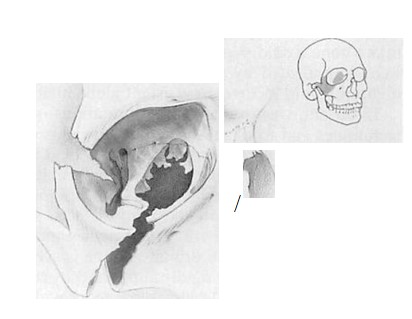 Figure 1. The typical orbital fracture that was encountered in this series is depicted schematically. From the illustration, it is possible to get a sense that a conventional orbital implant could not span the defect along the floor and medial wall and be securely positioned.
Figure 1. The typical orbital fracture that was encountered in this series is depicted schematically. From the illustration, it is possible to get a sense that a conventional orbital implant could not span the defect along the floor and medial wall and be securely positioned. 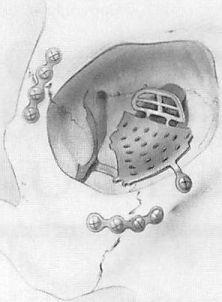 Figure 2. Schematic view of a custom orbital implant. After reduction and fixation of the orbital rims, the titanium implant is positioned and trimmed to span the defect. The edges of the implant are supported by the minimal intact bone along the orbital floor and medial wall.
Figure 2. Schematic view of a custom orbital implant. After reduction and fixation of the orbital rims, the titanium implant is positioned and trimmed to span the defect. The edges of the implant are supported by the minimal intact bone along the orbital floor and medial wall.
Results
Of the 22 orbital fractures treated by rigid internal orbital fixation, 11 were repaired using a custom metallic implant. Autologous bone grafts fixed to a mini/microplate were used in 7 cases and lag screw fixation of the bone grafts was applied in 4 orbits. Coexistent severe ocular injury in three of the cases required enucleation in the acute setting before the repair of the orbit.
Success of the surgical repair was determined subjectively by both the physicians and patient. A reoperation for significant persistent enophthalmos requiring additional bone graft orbital volume augmentation was required in only one case. Also, in one anophthalmic orbit, additional bone grafts were placed to achieve the desired orbital projection. There were no cases of overcorrection observed. No significant complications related to the orbital implants were encountered. Particularly, there were no cases of migration, infection, or extraocular muscle entrapment.
Case Reports
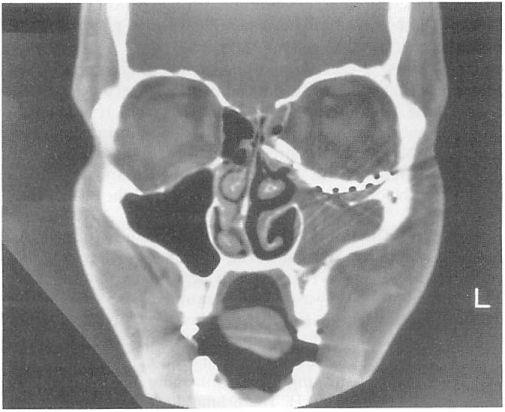
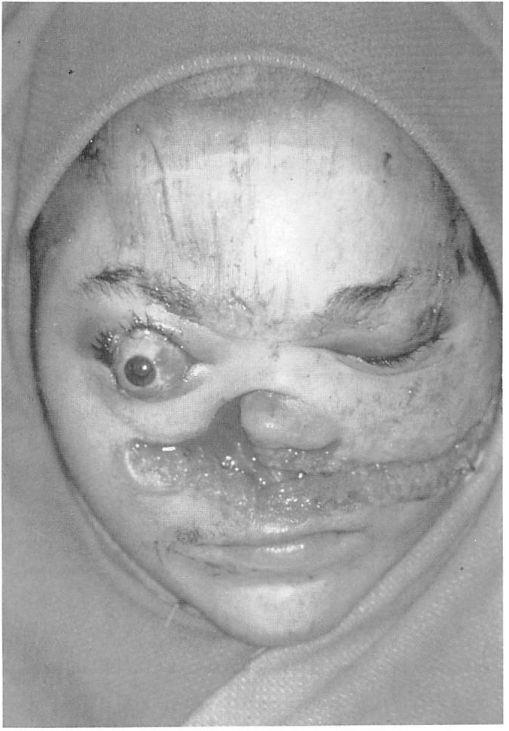
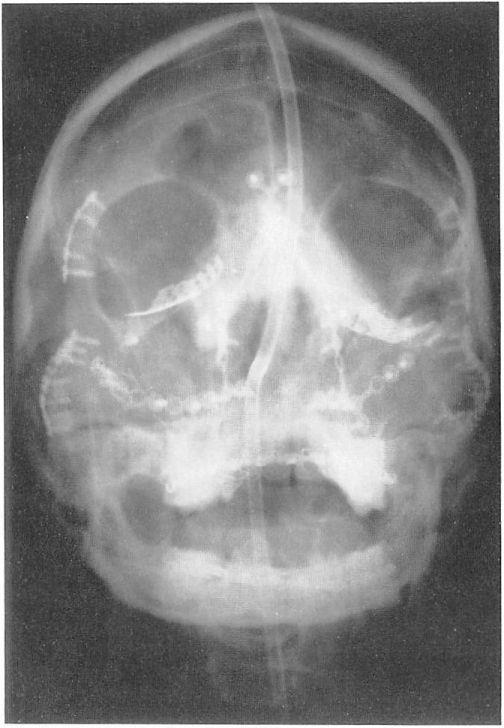
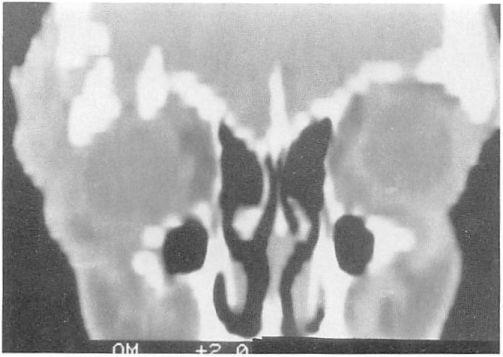
Case 1. A 23-year-old woman sustained a massive open panfacial fracture in a motor vehicle accident. There was gross distortion of the midface and orbital area and an avulsion of the right optic nerve (Fig 6). The preoperative computed tomography scan showed multiple comminuted facial fractures (Fig 7). The fractures were repaired acutely. Surgical exposure was achieved through bicoronal and subciliary incisions. The zygomatic, orbital, and maxillary structures were found to be 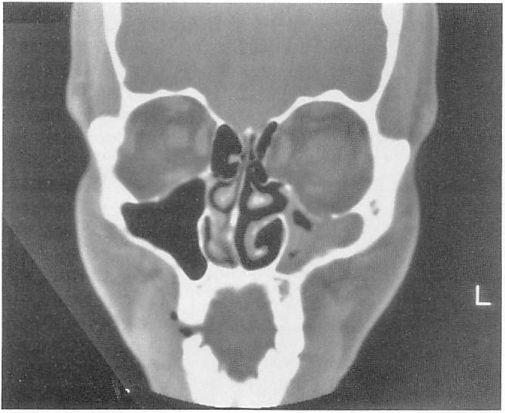 Figure 3. A preoperative coronal computed tomography appearance of a typical large orbital floor and medial wall defect.
Figure 3. A preoperative coronal computed tomography appearance of a typical large orbital floor and medial wall defect.
massively comminuted. Fragments of the orbital rim were repositioned anatomically, followed by manipulation of the zygomatic arches and maxillary buttresses into desired anatomic alignment. The large fragments were initially wired into position followed by fixation with titanium miniplates and screws. Traumatic telecanthus was then repaired by transnasal wiring technique. After repositing herniated orbital soft tissue, attention was directed at repairing the internal orbital skeleton. Since there was complete disruption of the lateral and medial walls and orbital floor bilaterally, orbital floor reconstruction was performed by trimming and shaping custom metallic orbital implants to cover each floor defect. Each titanium implant was fixed to the orbital rim with 1.5-mm diameter screws. The cantilevercd implant with wings extended medially and laterally, supported posteriorly by the intact portions of the orbital walls.
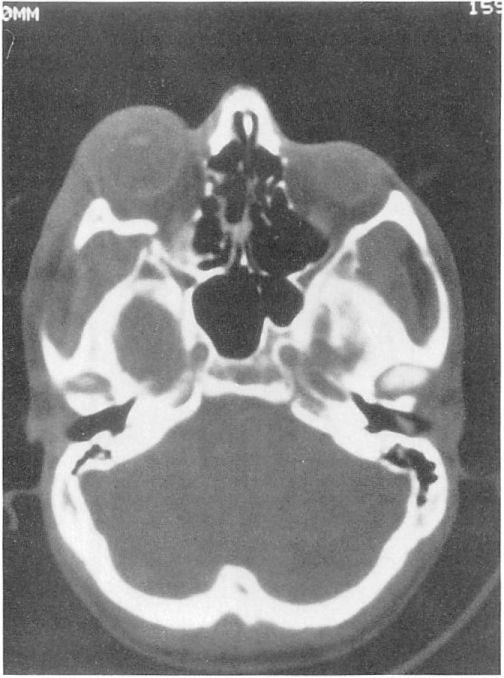
Figure 4. A postoperative coronal computed tomography scan of the fracture depicted in Figure 3. The custom mesh implant easily can be seen re-establishing the native contour of the orbital floor. A bone graft is supported by the medial portion of the floor implant and helps reconstitute the medial wall defect. 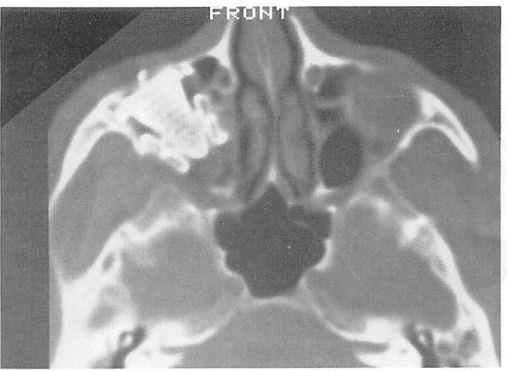 Figure 5. A representative postoperative axial computed tomography scan clearly depicts the custom-shaped orbital implant.
Figure 5. A representative postoperative axial computed tomography scan clearly depicts the custom-shaped orbital implant.
It served as a scaffold for outer calvarial bone grafts, which were placed on the implant to cover the remainder of the bony defect and to provide the desired orbital soft tissue projection. Postoperative plain films demonstrated the final positioning of the implant (Fig 8). The blinded, deviated right eye was fitted with a cosmetic scleral shell.
Figure 6. Case 1. Preoperative clinical appearance with open complex panfacial fracture, proptotic right globe, and avulsed right optic nerve.

Figure 7. Computed tomography scan of case 1 demonstrates bilateral comminuted complex orbital and facial fractures.
Figure 8. Case 1. Postreduction plain film depicts the presence of the internal orbital implants as well as the extensive amount of metallic implants that were required to repair the multiple facial and orbital fractures.Â
Figure 9. Case 1. Clinical appearance 2 years after surgery shows a scleral cosmetic shell in place over the right eye.
No additional surgery was necessary’. A 2-year follow-up examination demonstrated a good cosmetic result (Fig 9).
Case 2. A 22-year-old man was assaulted, sustaining a right complex orbital fracture, including the supraorbital area, zygoma, cranial base, and orbital floor. These fractures resulted in a proptotic entrapped globe and transmission of intracranial pulsations to the eye. The neurosurgical service performed a cra-niotomy to remove the damaged frontal lobe and to place a dural patch before commencement of repair of the orbital fractures.
Exposure of the orbital fractures was obtained through coronal and subciliary incisions. The orbital rims superiorly, laterally. and inferiorly were found to be severely comminuted. The internal orbit also was severely disrupted. There was a large defect in the orbital roof (Fig 10) with herniation of the anterior cranial fossa contents into the orbit resulting in a pulsatile globe. A large lateral wall defect was present with a 1.5-cm fragment that was displaced and impinged on the lateral rectus resulting in limited ductions (Fig 11). The orbital floor had a large defect laterally and posteriorly.
The superior, lateral, and inferior orbital rims were reduced anatomically, initially wired into position, and then fixated rigidly using miniplates. The orbital roof defect was reconstructed with
Figure 10. Case 2. Preoperative computed tomography. Coronal reconstruction shows the right orbital roof defect.
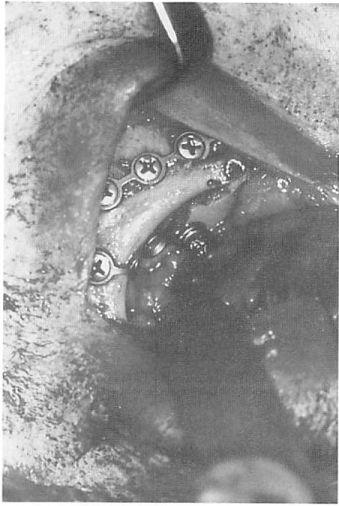
a cranial bone graft lag fixated with a 2-mm screw to the inner superior orbital rim. This resulted in an immobile bone graft that did not transmit the intracranial pulsations to the globe. The orbital floor defect was repaired using a bone graft that was fixated to a miniplate, cantilevered to span the floor defect, and anchored to the infraorbital rim with 1.5-mm diameter screws. This construct provided a stable platform to position additional bone grafts to cover the lateral wall defect (Fig 12).
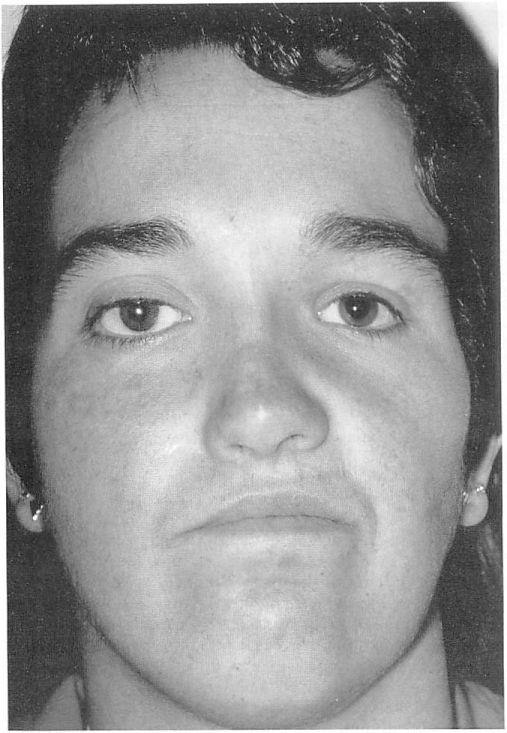
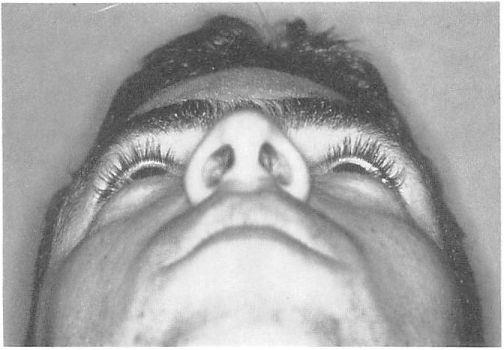
The 1-year postoperative results showed an excellent cosmetic result with resolution of the globe malposition (Fig 13), limited ductions, and globe pulsations.
Discussion
Over the past several years, there has been an increasing trend toward the early and complete repair of complex facial and orbital fractures.4-8 The improved results observed with this management can be attributed to the direct visualization and anatomic realignment of the fracture fragments using rigid fixation before the development of malunion of bony fragments. Miniplate fixation of the orbital/facial skeleton has been especially valuable in cases of complex fractures where there is severe comminution of the orbital rim.9 Recent uses of fine pliable yet strong meshed metallic implants have permitted application of rigid fixation to the internal orbit.10-11 Application of earlier intervention and rigid fixation has been helpful in reducing the most significant cause of postoperative enophthalmos— enlargement of the bony orbital volume.1-3-12
In this series of patients, the principles of benefits of rigid fixation of the external orbital skeleton were applied to the internal orbit. This technique was only applied in those cases where there was such massive comminution of the internal orbital walls that there was not a stable construct on which an implant could be positioned in a stable manner.
The vitallium mesh or custom orbital implants offers both pliability and strength permitting simple and precise adaptation to the contour of the orbital walls. Unlike other
Orbital Fracture Repair
fracture sites in the facial skeleton, the orbital floor is immobile and has no muscular insertions; therefore, it does not have to resist any significant shearing forces. Its only mechanical role is to confine and support the orbital soft tissue. For this reason, these orbital implants can be adequately supported with only one screw anchored at the orbital rim. Although the plates can provide support for the orbital soft tissue with only one point fixation, the goal of placement of the floor implant is to span the defect and establish continuity with the intact portion of the orbital vault. This most accurately restores the desired orbital volume and contour, reduces the chance of a free edge of the implant impinging on orbital soft tissue, and offers additional mechanical support for the implant.
Rigidly fixated bone grafts either through a lag screw or plate proved to be useful. This technique lacks some of the flexibility of sizing and contouring of custom metallic plates, but in selected cases it provides adequate rigid support of the orbital soft tissue while minimizing the alloplastic load.
The major goal of restoration of the orbital volume and structural integrity of the internal orbital walls is to prevent significant postoperative globe malposition. In this limited series biased toward the most severely traumatized orbits, this goal was achieved, for there was only one case of significant postoperative enophthalmos that required additional orbital augmentation surgery.
Figure 11. Case 2. Preoperative computed tomography. Axial view reveals comminuted, displaced right lateral wall fracture.
This is surprising since resolution of the acute soft tissue edema can result in a significant change in the globe position. For this reason. the intraoperative goal is to restore the internal orbital anatomy and achieve only a slight overcorrection to account for soft tissue swelling. Restoration of the rigid orbital anatomy should adequately address the globe position since the nonedematous soft tissue volume does not significantly change.1-3 Metallic implants used for support decrease the need for autogenous bone grafts and their inherent unpredictability due to variable resorption. Theoretically, the entire desired orbital skeletal contour could be achieved through an appropriately shaped custom metallic orbital implant. However, in practice, additional projection, particularly toward the apical region of the orbit, would necessitate curving the posterior free edge of the plate toward the optic nerve and other orbital apical structures. To avoid potential complications in this setting, it was decided to place bone grafts on the implant to achieve the desired orbital volume augmentation. Additionally, once fixated to the orbital rim, it is difficult to further manipulate the custom orbital implant, so fine- tuning of the orbital projection was achieved by placement of autologous implants.
Given the extensive injuries in these polytraumatized patients, further surgical intervention was commonly encountered. Additional orbital/oculoplastic procedures were required in five patients. These included correction of canthal and lid malposition, strabismus, and lacrimal obstruction.
Figure 12. Case 2. Intraoperative view of the bone graft fixated to a miniplate and anchored at the orbital rim.
Figure 13. Case 2. Appearance 3 months after surgery.
Of note, there have been no implant-related problems. Despite communication with the sinuses, no infections were observed. Migration, erosion, and entrapment, although theoretically possible, have not been encountered in our experience.
In cases where the orbit was reoperated, there was no difficulty encountered in elevating the periorbita from the plate, and there was no significant herniation of orbital contents through the implant’s fine mesh. Although not necessary in cases in this series, if removal of the implant is necessary, it can easily be accomplished after removing the screws securing the plate to the orbital rim.
Postoperative plain X rays were routinely obtained and documented the adequate reduction and plate position. Because titanium is less reflective than steel and nonmagnetic, useful images with computed tomography and magnetic resonance imaging can be obtained with the implants in place.
Autologous bone grafts, placed on the rigidly fixated internal orbital plate, were routinely used adjunctively to establish the desired orbital projection and to cover other defects, especially in the lateral and medial walls, that were not covered by the custom-shaped implant. Although not absolutely required, the placement of autologous bone, or any other implant, provides an additional barrier to further isolate the orbital soft tissue compartment from its adjacent structures.
References
1. Manson PN. Clifford CM. Su CT. et al. Mechanisms of global support and posttraumatic enophthalmos: I. The anatomy of the ligament sling and its relation to intramuscular cone orbital fat. Plast Reconstr Surg 1986:77:193— 20
2. Manson PN, Grivas A, Rosenbaum A, et al. Studies on enophthalmos: II. The measurement of orbital injuries and their treatment by quantitive computed tomography. Plast Reconstr Surg 1986;77:203-14.
3. Jackson IT. Classification and treatment of orbitozygomatic and orbitoethmoid fractures. The place of bone grafting and plate fixation. Clin Plast Surg 1989;16:77-91.
4. Antonyshyn O, Gruss JS, Galbraith DJ, Hurwitz JJ. Com-plex orbital fractures: a critical analysis of immediate bone graft reconstruction. Ann Plast Surg 1989;22:220-35.
5. Denny AD, Gonnering RS. Early repair of complex orbital fractures. Retina 1990;10(Suppl 1):S8—19.
6. Manson PN, Crawley WA, Yaremchuk MJ, et al. Midface fractures: advantages of immediate extended open reduction and bone grafting. Plast Reconstr Surg 1985;76:1-12.
7. Gruss JS, Mackinnon SE, Kassel EE, Copper PW. The role of primary bone grafting in complex craniomaxillofacial trauma. Plast Reconstr Suig 1985;75:17-24.
8. Markowitz BL, Manson PN. Panfacial fractures: organization of treatment. Clin Plast Surg 1989;16:105-14.
9. Jackson IT, Adham MN. Metallic plate stabilisation of bone grafts in craniofacial surgery. Br J Plast Surg 1986;39: 341-4.
10. Glassman RD, Manson PN, Vanderkolk CA, et al. Rigid fixation of internal orbital fractures. Plast Reconstr Surg 1990;86:1103-11.
11. Sargent LA, Fulks KD. Reconstruction of internal orbital fractures with Vitallium mesh. Plast Reconstr Surg 1991 ;88: 31-8.
12. Bite U, Jackson IT, Forbes GS, Gehring DG: Orbital volume measurements in enophthalmos using three-dimensional CT imaging. Plast Reconstr Surg 1985;75:502-8. 559