Microfixation of Acute Orbital Fractures
Microfixation techniques were used as an adjunct to the use of miniplates and screws in the acute treatment of fractures involving the orbit in 42 patients over a 2-year period. Miniplates were used in all fractures at the Le Fort I level and at the zygomatic- frontal suture in high-energy injuries. Microfixation was used to stabilize all other fractures of the zygomatic, nasoethmoid, and frontal areas. Problems with plate visibility and objectionable palpability through thin periorbital skin were eliminated. The use of microplates allowed more precise positioning of small fragments than possible with miniplates or interfragmentary wires. Fracture reduction remained clinically stable in the frontal and nasoethmoid areas. Microplates were inadequate to resist soft tissue deforming forces along the infraorbital rim and the zygomatic arch in high-energy injuries.
Yaremchuk MJ, Del Vecchio DA, Fiala TGS, Lee WPA. Microfixation of acute orbital fractures. Ann Plast Surg 1993;30:385-397
From the Division of Plastic Surgery, Department of Surgery, Massachusetts General Hospital and Harvard Medical School, Boston, MA.
Received Sep 4, 1991, and in revised form Jun 3, 1992. Accepted for publication Jun 19, 1992.
Address correspondence to Dr Yaremchuk, Massachusetts General Hospital, WACC 453, Boston, MA 02114.
Plate and screw fixation techniques have had a proven role in surgery of the craniomaxillofacial skeleton since their introduction almost 20 years ago. Plate and screw fixation systems have evolved into two types. Historically, larger scaled systems requiring bicortical placement of the screws and requiring external incisions for their placement were used for mandibular reconstruction [1, 2]. These plates are of sufficient strength to neutralize the powerful muscles of mastication, thereby minimizing or avoiding the need for maxillomandibular fixation (MMF) after surgery. Miniplates, which are considerably smaller, were introduced in 1973 by Michelet and colleagues [3] as a more “user-friendly†means of achieving rigid fixation of the mandible. These plates are more easily bent, use monocortical screws, and can be placed transorally. Although the stability achieved with minifixation of the mandible is somewhat controversial [4, 5], their application in the thin bones of the upper face has gained wide acceptance [6-9].
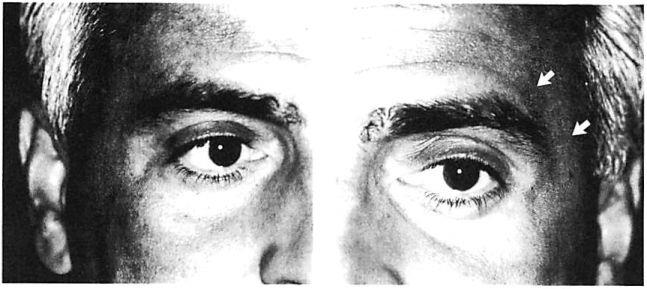
With experience, certain disadvantages of miniplate fixation of the mid and upper face have become evident. These have been related largely to scale, and include problems of palpability and visibility [10], especially around the orbit and forehead where the skin is thin (Fig 1). Sometimes these problems require a second operation for plate removal. Francel and associates [11] reviewed the incidence of miniplate removal in the treatment of 1,200 fractures in 507 patients managed in a trauma center setting. They found that 12% of all miniplates used subsequently required removal. Of this 12%, plate palpability or visibility prompted miniplate removal in 13%. In other words, between 1% and 2% of all miniplates placed were subsequently removed due to problems related to their prominence [11]. Review of our data reveals a similar incidence of plate removal for miniplate prominence in the treatment of 150 patients. Not considered in these statistics are patients who object to the prominence of their miniplates but are unwilling to undergo a second operation for their removal. Miniplates may be too large for the treatment of certain injuries. The hole spacing of miniplates may be too wide to fixate certain comminuted fractures. Plate configuration may also limit the contouring of miniplates and prevents ideal adaptation around the complex curvatures of the orbit.
Luhr [12] was the first to reduce the scale of his minifixation system. His microsystem was designed for use in the pediatric facial skeleton and has gained immediate acceptance by craniofacial surgeons for the correction of congenital deformities [13, 14]. Recently, Luhr [15] pointed out potential indications, whereas others [16] have reported their general satisfaction with the use of microfixation techniques in the adult facial skeleton.
Fig 1. Postoperative appearance of right and left orbital areas in a patient who underwent open reduction and internal fixation of complex facial fractures including fixation with a miniplate at the left zygomaticofrontal sulure. No surgery was performed in right zygomaticofrontal area. (A) Right zygomaticofrontal suture area, which did not undergo surgery. (B) Left zygomaticofrontal area. Arrows point to subtle contour of miniplate transmitted through thin skin envelope of lateral brow.
This report analyzes the use of microfixation techniques in the acute phase treatment of 42 consecutive patients with fractures involving the adult orbit. The reduced scale of the microplates made them ideally suited for use in the frontal and nasoethmoid areas. In the zygomatic area, microplates were effective when used with miniplates placed at the Le Fort I level for low- and moderate-energy level injuries. They provided insufficient stability along the infraorbital rim and zygomatic arch in high-energy injuries. Concerns related to their visibility or objectionable palpability were not encountered.
Material and Methods
The Microsystem
The microsystem used in this patient series has been the one designed by Luhr [12] (Howmedica, Rutherford, NJ). It is manufactured from vitallium (cobalt-chromium-molybdenum alloy). This system uses self-tapping screws having a cortical pitch (thread spacing) of only 0.3 mm and there-fore allowing use in extremely thin bone. Screw diameter is 0.8 mm. Plate thickness is 0.5 mm, with holes spaced at 4-mm intervals. The holes are joined by a straight connecting bar that allows three-dimensional plate bending without hole distortion. This size represents an —50% reduction in scale of most commercially available minisystems. Plates from the Luhr mandibular system, minisystem, and microsystem are presented for comparison in Figure 2.
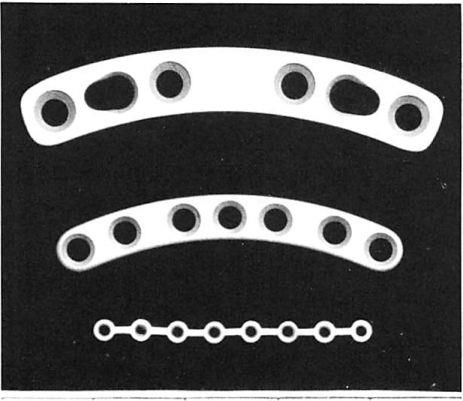 Fig 2. Plates from (top to bottom) the Luhr mandibuJar system, minisystem, and microsystem.
Fig 2. Plates from (top to bottom) the Luhr mandibuJar system, minisystem, and microsystem.
The use of the microsystem is more technically demanding than the use of its mini counterpart. Microfixation surgery uses exactly the same principles and techniques as its macro counterpart, but the smaller size allows for less operator error and demands meticulous instrument upkeep. We have found that the most important element in technique is maintaining a coaxial relationship between the drill hole, screw, and screwdriver during screw insertion. This technical error as well as failure to drill through the bone completely will lead to a high incidence of screw fracture. Loupe magnification (2.0-2.5X) is recommended.
Microfixation techniques were used in 42 patients treated for facial trauma involving the orbit, over a 16-month period from January 1989 to April 1990. The majority of injuries resulted from motor vehicle accidents (70%) or personal assaults (25%). Patients ranged in age from 14 to 74 years with a mean age of 29 years. There were 28 males and 14 females. Patient injury, method of treatment, and postoperative result were analyzed by retrospectively evaluating clinical records, pre and postoperative radiographic studies, as well as the patient follow-up examination. Follow-up ranged from 6 months to 2 years (mean, 1 yr).
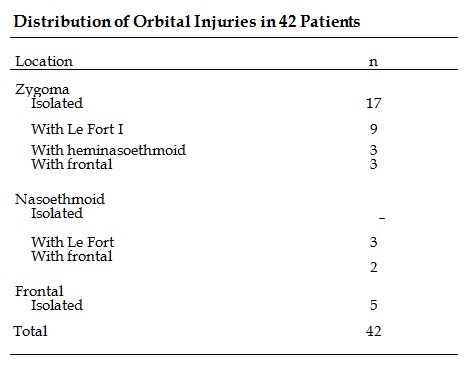
To categorize the injuries, the orbit was divided into the zygomatic, nasoethmoid, and supraorbital/frontal areas. The distribution of injuries is presented in the Table.
Surgical Technique
Before surgery, injuries were evaluated by careful physical examination and by computed tomographic (CT) scans. Exposure was obtained as appropriate using the gingivobuccal sulcus incision, subciliary skin muscle flap, lateral brow, coronal, and when available, preexisting lacerations. As described by Gruss and MacKinnon [17] and Manson and co-workers [18], subperiosteal dissection of all fracture sites was performed, and the fracture sites were then aligned anatomically, their position sometimes temporarily stabilized with interfragmentary wires or microplates, and when the desired three-dimensional relationship of the fragments was achieved, then fixated with plates and screws. Bone defects of >0.5 cm were bridged with cranial bone grafts that were wedged into place or fixated with a screw to a free hole of a plate.
The amount and type of fixation was determined by the nature of the fracture, the stability of adjacent structures, and the potential effect of masticatory forces. In general, miniplates were used for fixation at the four buttresses at the Le Fort I level and at the zygomaticofrontal articulation when there was wide separation at that area in panfacial or in high-energy Le Fort injuries. Otherwise, fixation in the supraorbital/frontal, zygomatic, and nasoethmoid areas was obtained with microplates.
Supraorbital / Frontal
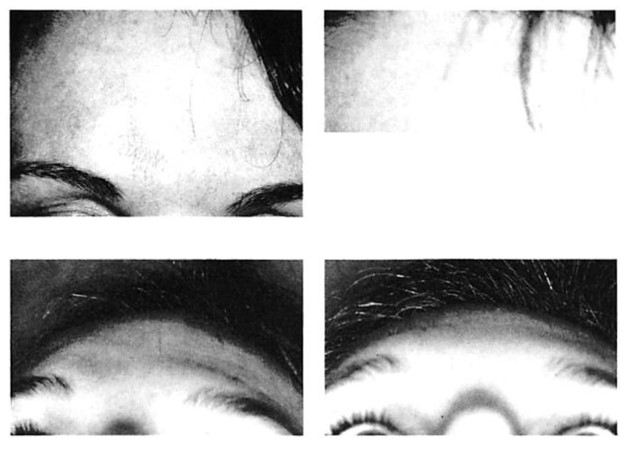
Long microreconstruction plates are ideal for fixation of the supraorbital rim and the anterior wall of the frontal sinus (Figs 3, 4) [19]. When segments are too small to be replaced, cranial bone grafts harvested from the outer table in the parietal area or from the inner table of cranial bone flaps are used as interposition or onlay grafts and are fixated with microplates and screws. Supraorbital detail can be restored precisely using onlay grafts lag-fixated with microscrews. These stabilized grafts are then contoured exactly with a high-speed contouring burr [19, 201- Countersinking avoids any potential problem with screw head protrusion if significant graft resorption should occur.
Zygomatic
Zygoma fractures were treated on the basis of segmentation and displacement, which can be predicted by preoperative CT scans and has been classified as low, medium, and high [21]. Low- energy zygoma fractures are those with little or no displacement and are incomplete through at least one articulation, most often at the zygomaticofrontal suture. When displacement was severe enough to warrant open reduction and internal fixation, fixation was accomplished with a mini-plate at the zygomaticomaxillary buttress to resist the pull of the masseter and with a microplate to maintain alignment at the infraorbital rim (Fig 5). Middle-energy zygoma fractures have complete fractures at all buttresses, varying degrees of comminution usually at the zygomaticomaxillary buttress, and mild to moderate displacement. After reduction, minifixation was used at the zygomaticomaxillary buttress, and microfixation at the zygomaticofrontal suture and infraorbital rim (Fig 6).
Fig 3. Isolated fracture of anterior wall of frontal sinus in patient with extremely thin soft tissue envelope and prominent frontal sinuses, who was treated with open reduction and internal fixation using microplates and screws. (A) Preoperative frontal view. (B) Postoperative frontal view \ year after surgery shows stable restoration of frontal sinus contour. (C) Preoperative worm’s eye view. (D) Postoperative worm’s eye view. (E) Intraoperative view from above after reduction and fixation with microplates and screws shows extremely low profile of system.
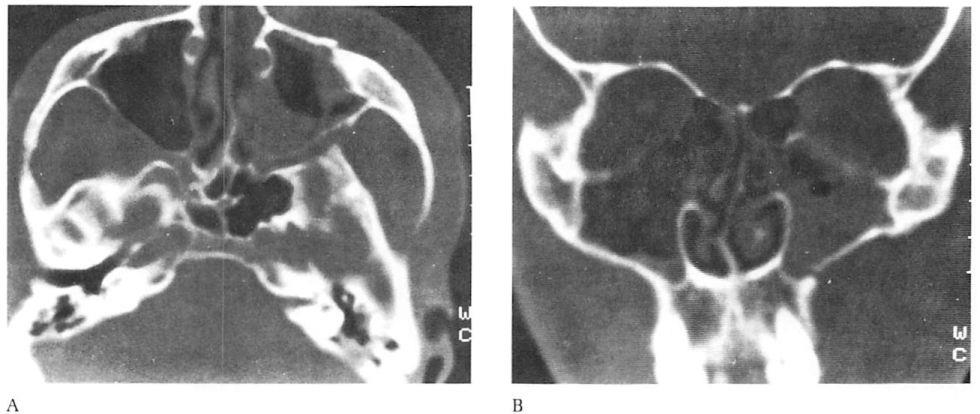
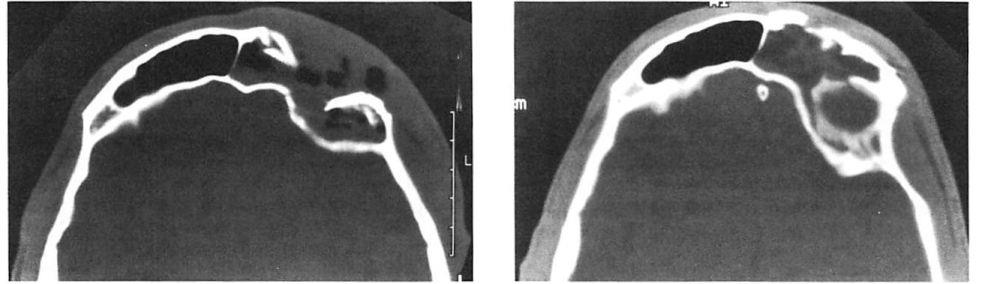 Fig 4. Highly comminuted fracture of supraorbital portion of large frontal sinus that extends to lateral orbit treated with open reduction and microplate and screw fixation. (A) Preoperative axial computed tomographic (CT) scan. (B) Postoperative axial CT shows stable reduction 2 months after injury. Note symmetrical contour of frontal soft tissues.
Fig 4. Highly comminuted fracture of supraorbital portion of large frontal sinus that extends to lateral orbit treated with open reduction and microplate and screw fixation. (A) Preoperative axial computed tomographic (CT) scan. (B) Postoperative axial CT shows stable reduction 2 months after injury. Note symmetrical contour of frontal soft tissues.
High-energy zygoma fractures usually occur in combination with Le Fort or panfacial injuries. They exhibit comminution in the lateral orbit as well as lateral displacement and posterior segmentation of the zygomatic arch.
In these injuries we have found that microplates are inadequate to overcome deforming forces from the overlying contused, swollen soft tissue envelope and muscle spasm (Fig 7). Their inability to maintain reduction may be obvious at the time of surgery. Sufficient miniplate fixation is crucial in these injuries. In addition to stabilizing the maxillary buttress at the Le Fort I level,
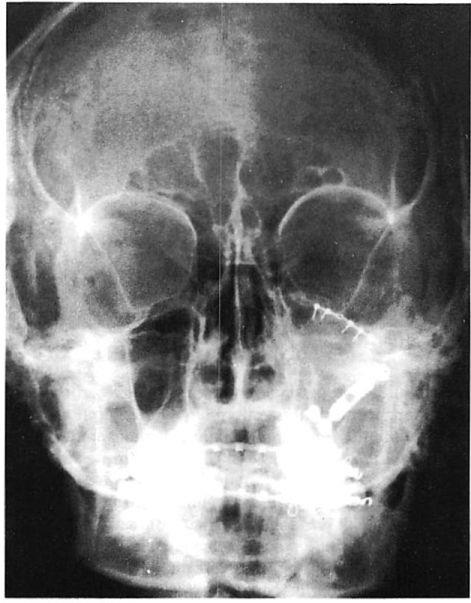
Fig 5. Low-energy zygoma fracture treated with mini- and microfixation. (A) Preoperative axial computed tomographic (CT) scan shows malar displacement. (B) Preoperative coronal CT scan shows slight displacement at zygomaticomaxillary buttress and no displacement at zygomaticofrontal articulation. (C) Postoperative plain film shows miniplate fixation at zygomaticomaxillary buttress and microplate fixation at the infraorbital rim. (Arch bars were used for maxillomandibular fixation to treat associated subcondylar fracture.)
miniplates are used for stabilization at the zygo-maticofrontal suture and along the zygomatic arch. Depending on the severity of the fracture, miniplate stabilization may also be necessary along the infraorbital rim. Microplates do have an important role in the temporary stabilization of these fractures. Unlike miniplates, microplates can be used to stabilize extremely small fragments. Because they can be bent manually after they have been applied, a temporary “best guess†reduction and fixation can be altered to allow reduction at another disrupted articulation. After reduction of the entire complex is achieved, it is then stabilized by applying miniplates.
Nasoethmoid
Markowitz and associates |22) have defined the importance and management of the canthal bearing segment in nasoethmoid orbital fractures. Plate and screw fixation is used to stabilize the projection of the frontal bone, nose, and superior and inferior orbital rims. We abide by their guidelines, which will not be repeated here. Microfixation is used in this area exclusively after anatomical reduction of fracture segments and after temporary interfragmentary wire stabilization (Fig 8).
Fig 6. Middle-energy zygoma fracture treated with miniarid microfixation. (A) Preoperative axial computed tomographic (CT) scan shoivs malar displacement and buckling of lateral orbital wall. (B) Preoperative coronal CT scan shows comminution at zygomaticomaxillary buttress and displacement at zygomaticofrontal articulation. There is slight bowing of the zygomatic arch. (C) Postoperative plain film shows microplate at zygomaticofrontal suture area and rim with miniplate at the zygomaticomaxillary buttress. Surgery was performed through a subciliary and gingivobuccal sulcus incision. The arch shape was restored with external pressure.
Microplates or microscrews are used to stabilize onlay or cantilever dorsal nasal bone grafts. A microscrew fixated to the medial orbital rim in the supratrochlear area provides an excellent place for fixation of transnasal wires used to maintain reduction of the canthal bearing bone segment.
Results
In this series only 1 patient had clinically apparent loss of fracture reduction in the area stabilized by microplates (see Fig 4). Of the 42 patients, 23 had CT scans in the early postoperative period and, with the exception of the patient presented in Figure 4, revealed near anatomical reduction of their fractures. There were 2 patients who required secondary surgery to improve globe position as a result of inadequate initial internal orbit reconstruction.
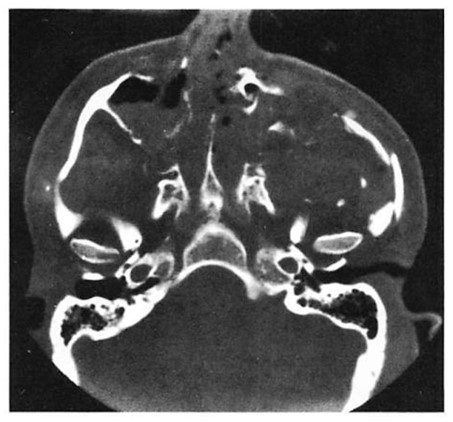
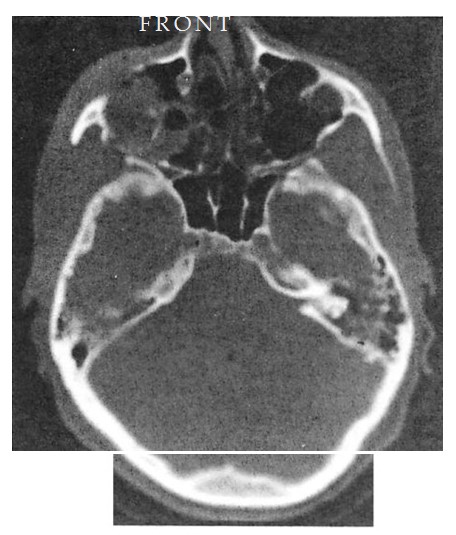
Fig 7. Very high energy Le Fort injury with open crush injury on the left side. Miniplates were used for fixation at maxillary buttresses and zygomaticofrontal sutures. Microplates were used along infraorbital rim and along the zygomatic arch on both sides. Computed tomographic (CT) scan performed 48 hours postoperatively shows loss of infraorbital rim projection on the severely comminuted left side and good projection on less severely injured right side. (A) Preoperative coronal CT shows pronounced lateral displacement of the zygoma on the left side. (B) Preoperative axial CT shows comminution and telescoping of left zygomatic arch. (C) Postoperative CT at 48 hours shows infraorbital rim and malar and arch collapse on left side.
Two patients who suffered Le Fort fractures developed infection. One had had a lateral orbital and a transverse nasal laceration repaired in the emergency room on an urgent basis. Fracture reduction was performed using these lacerations as partial exposure 48 hours later. Six days after injury and 4 days postoperatively, local infections were drained that overlay a microplate at the zygomaticofrontal suture area and a micro- screw used to fixate a nasal bone graft. This was treated with drainage and local dressings as well as oral antibiotics. The areas remained healed and stable at 1-year follow-up.
The patient presented in Figure 4 also had an open wound with extensive soft tissue injuries that were sutured in the emergency room. The patient developed extensive necrosis of the tem-poralis requiring debridement and intravenous antibiotic therapy. Six weeks later this patient presented with orbital cellulitis. Debridement at this time revealed further muscle necrosis and loose microfixation hardware, which was removed and replaced with miniplates after appropriate debridement. A secondary reconstruction was performed 6 months after the initial surgery without incident.
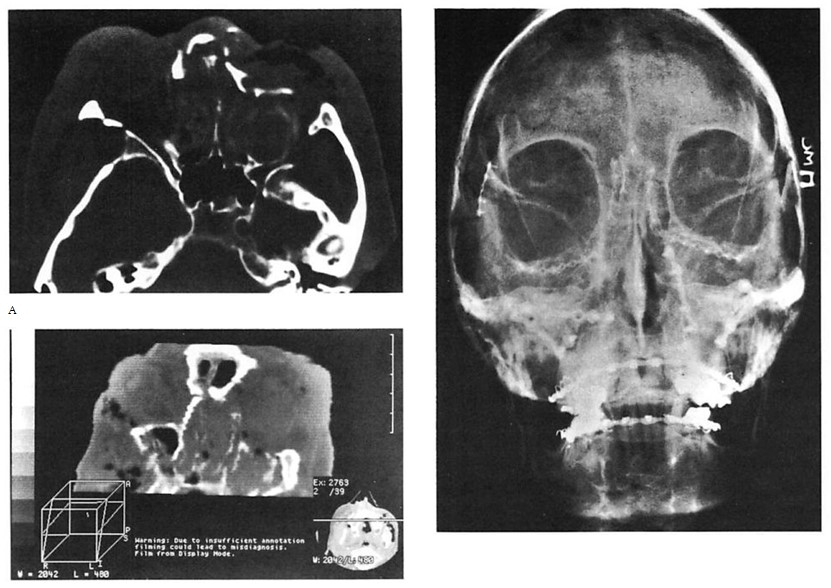
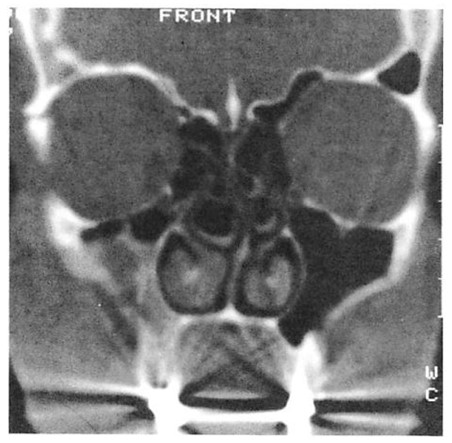
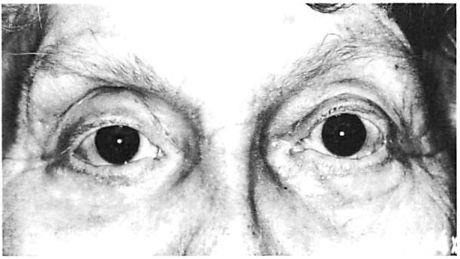 Fig 8. Comminuted nasoethmoid orbital and Le Fort fractures managed in a multiply injured 82-year-old woman. (No internal orbit reconstruction was performed.) (A) Preoperative axial computed tomographic (CT) scan. (B) Preoperative coronal reconstruction shows displacement of medial orbital walls. (Cervical-spine injuries precluded positioning for coronal scan.) (C) Postoperative coronal view (reconstructed) at 4 weeks shoivs stable reduction of medial orbital walls. (D) Postoperative plain film shows fixation used. (E) Clinical result 6 months postoperatively.
Fig 8. Comminuted nasoethmoid orbital and Le Fort fractures managed in a multiply injured 82-year-old woman. (No internal orbit reconstruction was performed.) (A) Preoperative axial computed tomographic (CT) scan. (B) Preoperative coronal reconstruction shows displacement of medial orbital walls. (Cervical-spine injuries precluded positioning for coronal scan.) (C) Postoperative coronal view (reconstructed) at 4 weeks shoivs stable reduction of medial orbital walls. (D) Postoperative plain film shows fixation used. (E) Clinical result 6 months postoperatively.
No microplates have required removal because of visibility or objectionable palpability.
Discussion
Miniplate fixation of complex facial fractures has been considered superior to wire osteosynthesis because it allows precise three-dimensional positioning of fracture segments and better stability to resist soft tissue-deforming forces of mastication and scar contracture. In so doing, it provides the potential for avoiding MMF and decreasing convalescence while providing a superior aesthetic result [23-29]. Wire osteosynthesis is less stable because wires stretch and because they provide less axial rigidity than plate fixation [30]. At present, there is no objective clinical evidence to prove the long-term stability of miniplate over wire osteosynthesis. Quite reasonably, trauma surgeons extrapolate the objective data from the orthognathic literature, which shows a superiority of rigid fixation techniques [7, 31-38], to confirm their clinical impressions. Except for the obvious conclusions that the smaller size of microfixation systems provides more flexibility in contouring, allows fixation of smaller fracture segments, and avoids problems of visibility and objectionable palpability, the important issue is whether microfixation systems provide sufficient stability of reduced fracture segments.
Presently, Luhr’s torque load data [12] is the only information available regarding the biomechanical attributes of microfixation systems. He compared the maximum torque load that can be applied before the screw is stripped in the hole between mini- and microscrews. These data showed only a small difference between pretapped (2 mm) mini- and self-tapping microscrews (0.8 mm).
The biomechanical testing of multiple configu-rations of miniplates and wire fixation of simu-lated zygoma fractures, by Davidson and co-workers [39], provides some perspective for evaluating the stability of microfixation used in combination with minifixation for facial skeletal fractures. His group analyzed different methods of internal fixation of simple displaced fractures of the zygoma in a cadaver study. The experimental conditions would most closely resemble the clinical situation of a moderate-energy zygoma fracture [21]. Various modes of fixation using interfragmentary wires and miniplates were used. They subsequently classified the different methods of internal fixation into the following three groups: (1) stable, (2) acceptably stable, and (3) unstable. These were defined by the average net rotational displacement obtained when tested with loads simulating those placed on the zygoma in vivo. Stable fixation was shown by those methods that allowed <2 degrees of net rotational displacement (1 mm of displacement at any one of the articulations), acceptably stable fixation allowed ^5 degrees of net rotational displacement (^15 mm), and unstable fixation showed >5 degrees of net rotational displacement (>15 mm). Comparing the fixation techniques used in this article with those studied by Davidson and his group [39] sheds some light on the stability of our mini/micro techniques. We have advocated placing miniplates at the zygomaticomaxillary buttress and microplates at the infraorbital rim and zygomaticofrontal suture as necessary for moderate-energy injuries. Davidson [39] found that a miniplate at the lateral buttress and a wire at the infraorbital rim provided acceptably stable fixation. He found stable fixation with a miniplate at the buttress and wires at the infraorbital rim and zygomaticofrontal suture, or with a single wire at the zygomaticofrontal suture in combination with the buttress miniplate. Assuming microplate fixation is at least as stable as interfragmentary wiring, these data would suggest that our combination of a miniplate at the lateral buttress and microplates at the orbital rims is stable as defined by Davidson and his group [39].
Previous efforts in calculating and analyzing stress-strain patterns in the facial skeleton have centered on the mandible. By likening the mandible to a loaded cantilevered beam, classical mechanical analysis has been used to estimate flexion patterns caused by muscles acting on the mandible. Generally, the masseter muscle is considered to contribute the most significant pull on the mandible; the magnitude of this force can be directly measured. Modeling similar stress-strain patterns in the midface is considerably more complex, due to the three-dimensional shape of the midfacial skeleton and the multiplicity of muscle force vectors acting at different points on the bony surface. Thus, to date, it has not been possible to create an accurate model for midfacial mechanical analysis [40].
Conventional mechanics, however, may be used in a limited way to assess choice of fixation hardware in the midfacial region.
Likening the fixation plate to a cantilevered rectangular beam is the basis of this analysis. The beam is fixed at one end, representing the stable side of the facial skeleton, and is free to move at the other “fractured†end. Because soft tissue- deforming forces, which tend to bend the beam, are distributed over a wide area rather than a single idealized point, a model in which bending forces are evenly distributed over the beam is used. In fact, muscular forces may be irregularly distributed over the beam rather than evenly distributed. This considerably complicates the model, requiring advanced differential equations for a solution, and is beyond the scope of this discussion.
The following equation for this model is given in standard engineering texts [41]:
Maximal deflection = Fsin0L4/(8 • E • I) (1)
Theta (0) is the angle between the long axis of the beam and the applied force (which, for simplicity, is assumed to act in a uniform direction over the length of the plate). L represents the lever arm length, F is the applied force per unit length, E is the elastic modulus of the material, and I is the moment of inertia of the beam.
In the fracture model, L corresponds to the length of the fractured segment. E, the elastic modulus, is an inherent property of both the material and the process used in the manufacture of the fixation device. I, the moment of inertia, is the factor that introduces the effects of plate size and shape into the bending equation.
Notice that the length of the fixation plate is not directly found in this equation. Longer plates are beneficial, as they permit screw fixation at an increased distance from the fracture site. This reduces the chance of screw pullout, as the torque exerted by adjacent soft tissues is spread out over the increased plate length, resulting in smaller forces for the screws to counteract. Thus, in a situation where a short plate is apt to fail due to screw pullout, a longer plate length is more likely to provide stable fixation. Plate length, therefore, should be chosen based on the expected torque exerted on the fixation plate.
Because bone healing and fracture stability depend directly on immobilization of the fracture, strategies that minimize movement are of importance. These include the following:
(1) Decrease F (the distractive force) by means of muscle immobilization, which may be possible through the use of MMF.
(2) Use plates with larger moments of inertia, which may be achieved in two ways, i.e., either by using single plates of increased dimensions or by the application of multiple plates. In the former scheme, if the fixation plates are likened to a solid rectangular beam of height (a) and width (b), the moments of inertia (I) about the neutral axis (as used in Eq 1) are as follows:
Ix = a3b/12 and Iy = ab3/12 (2)
The moment of inertia is proportional to the cube of the thickness of the plate, tending to resist the bending moment. Thus, increasing plate thickness by 10% in the appropriate dimension results in a reduction of lateral bending by 25%.
Use of multiple plates also increases the effective moment of inertia. Placing two plates side by side doubles the effective plate width, decreasing deflection by 50%. Similarly, stacking plates one atop another has an identical effect. A small degree of slippage between stacked plates prevents the eightfold reduction of bending one would obtain with a single plate of doubled thickness (R. M. Rose, personal communication). Increasing the scale of plates, of course, increases the likelihood for objectionable palpability or visibility.
There is yet another drawback to using increasingly larger plates. Because the elastic modulus of the plate is much higher than the adjacent bone (usually 10-15-fold) [42], the fixation device bears most of the stresses transmitted through the repaired segment. This is known as “stress shielding.†As a consequence of Wolff’s law, disuse osteopenia occurs in the bone under the fixation plate and immediately adjacent to the ends of the fixation plate [42].
An ideally sized implant, therefore, must allow appropriate mechanical stability for initial fracture healing, be designed to avoid fracture failure, but minimize adverse effects from stress shielding.
(3) Increase the elastic modulus of the material used in the manufacture of the fixation plate. Vitallium has an elastic modulus approximately double that of the titanium alloy used in surgical
implants, making vitallium plates twice as rigid as titanium ones. Thus, deflection caused by soft tissue-deforming forces can be expected to be reduced by 50% if vitallium plates are used instead of titanium ones of equal size and shape. Conversely, if the thickness of a titanium plate were increased ~25%, this enlarged plate would have the same flexural rigidity (El product) as the initial vitallium plate.
(4) Apply fixation plates optimally. According to mechanical analysis based on fixation of long bones, when approximation of the fracture ends is good, fixation plates should be applied in the “plane of greatest tension†[42]. The plate thus acts as a “tension band,†and the bending moment across the fracture site tends to compress the fracture for optimal healing, even when specially designed compression plates are not used. Additionally, the plate should be tightly fastened to the bone to avoid bending stresses on the screws, which are poorly tolerated.
With poor apposition of the fracture ends, the plate alone must bear the bending moment. According to Radin and associates [42], the typical plate has <1% of the rigidity of the combined bone-plate system. In cases of poor apposition, plates should be placed so their width, which is usually greater than plate thickness, resists the bending moment. By placing the plate at right angles to the plane of maximum tension in these situations, increased flexural rigidity can be obtained. This arrangement, however, subjects the screws to increased bending and torsional forces, increasing the risk of screw failure. Additionally, when significant bony gaps exist, the use of multiple plates and/or bone grafting should be considered, as it results in a significantly more rigid fixation arrangement.
L, the lever arm distance, is largely determined by fracture anatomy. Because overall deflection is proportional to the fourth power of this distance, this parameter plays a central role in determining the chance of success of a given fixation arrangement. For example, in the zygoma, a fracture at the zygomaticomaxillary suture would be associated with a large value of L, and hence L4, compared with other zygomatic fractures. Unless reinforcing strategies, such as using larger plates, were used, failure of fixation would theoretically be most likely at this location. This corresponds with the empirical observation that fractures involving the lateral buttress need miniplate fixation for successful stabilization.
In short, multiple factors contribute to determine whether a given repair is mechanically stable. At present, a model of fracture stability in the midface and orbital regions, reflecting these multiple factors, does not exist. Thus, clinical experience, guided by an understanding of physical principles, remains of paramount importance in the treatment of these fractures.
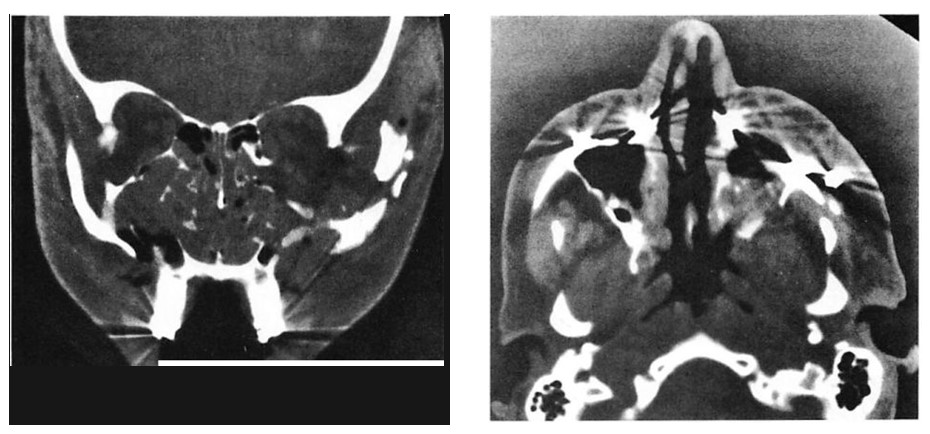
As noted previously, our clinical experience supports the use of microfixation techniques alone in the frontal and nasoethmoid areas as well as adjunctively with the use of miniplates in certain zygomatic and Le Fort injuries. Postoperative CT scans showing anatomical reduction of fracture segments assumes that anatomical and not “overreduction†was performed at surgery and that bone position will not deteriorate with time. In our opinion, these are safe assumptions. However, objective evidence of the stability of these fixation techniques would require documentation of bone position in the immediate postoperative period and again after bone healing had occurred. Such documentation is provided in Figure 9 for a patient who was treated for a moderate-energy Le Fort fracture by using miniplate fixation at the maxillary buttresses and microplate fixation along the infraorbital rims. Three patients in this series have been similarly documented showing stable bone position over time using the fixation techniques advocated here.
Summary
Microfixation techniques have been used in com-bination with miniplates in the treatment of facial fractures involving the orbit in 42 patients. Problems of scale resulting in objectionable palpability and visibility in the thin periorbital skin have been eliminated using microfixation techniques. By clinical analysis, selective use of microfixation as an adjunct to minifixation has not compromised stability of the reduction. The low incidence of infection in this series and available related biomechanical data [39] also suggests that adequate stability was obtained. The reduced scale and the three-dimensional conformability of microfixation systems provides the potential for improved results in orbital reconstruction.
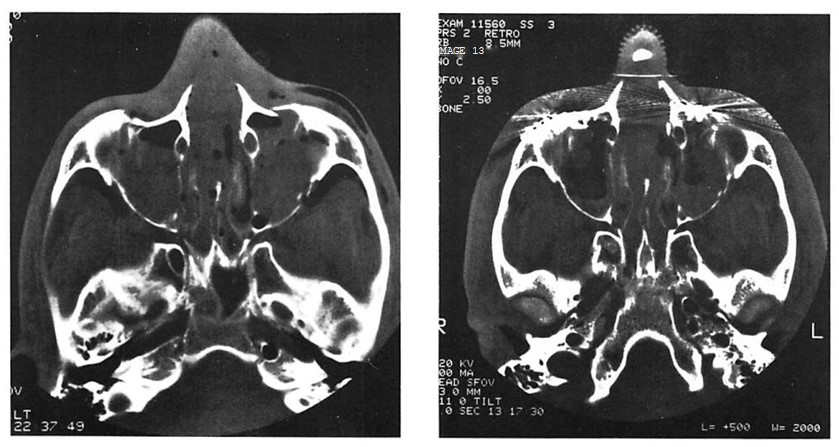

Fig 9. Computed tomographic (CT) scans of patient who suffered low-energy Le Fort II and III fractures treated with miniplates at the Le Fort I level and microplates along the infraorbital rims. (A) Preoperative CT shows pronounced impaction of central midface. (B) Axial scan through infraorbital rim shows anatomical reduction 3 days postoperatively. (C) CT scan at I year at similar cut shows unchanged position of bone fragments after healing.
We thank Professor R. M. Rose. ScD, PEng, of the Department of Materials Science and Engineering, Massachusetts Institute of Technology, for reviewing the biomechanical aspects of this paper.
Presented at the Northeastern Society of Plastic Surgeons 7th Annual Meeting, Bolton Landing, NY, September 14, 1990.
References
1. Luhr HG. Zur stabilen osteo synthese bei unter kiefer frakturen. Dtsch Zahnarztl Z 1968;23:754-762
2. Spiessl B. Rigid internal fixation of fractures of the lower jaw. Reconstr Surg Traumatol 1972;13:124-141
3. Michelet FX, Deymes ), Dessus B. Osteosynthesis with miniaturized screwed plates in maxillofacial surgery. J Maxillofac Surg 1973;1:79-88
4. Raveh J, Vuiliemin T, Laddrach K, et al. Plate osteosynthesis of 367 mandibular fractures. J Craniomaxillofac Surg 1987;15:244-251
5. Becker R. Stable compression plate fixation of mandibular fractures. Br J Oral Surg 1974;12:13-21
6. Champy M, Lodde AW, Wilk A, Grasset D. Plate osteosyn-thesis in midface fractures and osteotomies. Dtsch Z Mund Kiefer Gesichts Chir 1978;2:26-36
7. Rosen HM. Miniplate fixation of Le Fort I osteotomies. Plast Reconstr Surg 1986;78:748-754
8. Beals SP, Munro IR. The use of miniplates in craniomax- illofacial surgery. Plast Reconstr Surg 1987;79:33-38
9. Ewers R, Harle F. Experimental and clinical results of new advances in the treatment of facial trauma. Plast Reconstr Surg 1985;75:25-31
10. Marsh JL. The use of the Wurtzberg system to facilitate fixation in facial osteotomies. Clin Plast Surg 1989;16: 49-60
11. Francel TJ, Birely BC, Ringelman PR, Manson PN. The fate of plates and screws after facial fracture reconstruction. Plast Reconstr Surg 1992;90:568-573
12. Luhr HG. A microsystem for cranio-maxillofacial skeletal fixation. Preliminary report. J Craniomaxillofac Surg 1988; 16:312-314
13. Munro IR. Rigid fixation of facial osteotomies. Clin Plast Surg 1989;16:665-676
14. Sadove AM, Eppley BL. Microfixation techniques in pediatric craniomaxillofacial surgery. Ann Plast Surg 1991; 27:36-43
15. Luhr HG. Indications for use of a microsystem for internal fixation in craniofacial surgery. J Craniofac Surg 1990;1: 35-42
16. Eppley BL, Sadove AM. Application of microfixation techniques in reconstructive maxillofacial surgery. J Oral Maxillofac Surg 1991;49:683-688
17. Gruss JS, MacKinnon SE. Complex maxillary fractures: role of buttress reconstruction and immediate bone grafts. Plast Reconstr Surg 1986;78:9-22
18. Manson PN, Crawley WA, Yaremchuk MJ, et al. Midface fractures: advantages of immediate extended open reduction and bone grafting. Plast Reconstr Surg 1985;76:1-10
19. Yaremchuk MJ, Manson PN. Rigid fixation of frontal bone fractures. In: Yaremchuk MJ, Gruss JS, Manson, eds. Rigid fixation of the craniomaxillofacial skeleton. Boston: Butterworth-Heinemann, 1992
20. Shaw KE, Jackson IT, de al Pinal Mattoras F. In situ contouring of cranial bone grafts. Eur J Plast Surg 1987; 10:144-148
21. Manson PN, Markowitz B, Mirvis S, et al. Toward CT- based facial fracture treatment. Plast Reconstr Surg 1990; 85:202-212
22. Markowitz BL, Manson PN, Sargent L, et al. Management of the medial canthal tendon in nasoethmoid orbital fractures: the importance of the central fragment in classification and treatment. Plast Reconstr Surg 1991;87:843- 853
23. Antonyshyn O, Gruss JS. Complex orbital trauma: the role of rigid fixation and primary bone grafting. Adv Ophthalmol Plast Reconstr Surg 1985;7:61-72
24. Gruss JS, Phillips JH. Complex facial trauma: the evolving role of rigid fixation and immediate bone graft reconstruction. Clin Plast Surg 1989;16:93-104
25. Jackson IT, Somers PC, Kjar JG. The use of Champy miniplates for osteosynthesis in craniofacial deformities and trauma. Plast Reconstr Surg 1986;77:729-736
26. Jackson IT. Classification and treatment of orbitozygo- matic and orbitoethmoid fractures: the place of bone grafting and plate fixation. Clin Plast Surg 1989;16:77-91
27. Klotch DW, Gilliland R. Internal fixation versus conventional therapy in midface fractures. J Trauma 1987;27: 1136-1145
28. Rohrich RJ, Watamull D. Superiority of plate fixation in the management of zygoma fractures: long-term followup and evaluation. Presented at the 38th Annual Scientific Meeting of the American Society of Plastic and Reconstructive Surgeons, San Francisco, CA, October 31,1989
29. Schilli W, Ewers R, Niederdellmann H. Bone fixation with screws and plates in the maxillofacial region. Int J Oral Surg 1981;10(suppl l):329-342
30. Manson PN. Discussion of: Rinehart GC, Marsh JL, Hem- mer KM, and Bresina S. internal fixation of malar fractures: an experimental biophysical study. Plast Reconstr Surg 1989;84:26-27
31.Drommer R, Luhr HG. The stabilization of osteotomized maxillary segments with Luhr mini-plates in secondary cleft surgery. J Maxillofac Surg 1981;9:166-172
32. Harsha BC, Terry BC. Stabilization of Le Fort I osteotomies utilizing small bone plates. Int J Adult Orthod Orthog Surg 1986;1:69-78
33. Horster W. Experience with functionally stable plate os-teosynthesis after forward displacement of the upper jaw. J Maxillofac Surg 1980;8:176-184
34. Jeter TS, Van Sickels JE, Dowlick MF. Modified techniques for internal fixation of sagittal ramus osteotomies. J Oral Maxillofac Surg 1984;42:270-272
35. Paulus GW, Steinhauser EW. A comparative study of wire osteosynthesis versus bone screws in the treatment of mandibular prognathism. Oral Surg Oral Med Oral Pathol 1982;54:2-11
36. Posnick JC, Ewing MP. Skeletal stability after Le Fort I maxillary advancement in patients with unilateral cleft lip and palate. Plast Reconstr Surg 1990;85:706-710
37. Van Sickels JE, Flanary CM. Stability associated with mandibular advancement treated with rigid osseous fixation. J Oral Maxillofac Surg 1985;43:341-348
38. Van Sickels JE, Larsen AJ, Thrash WJ. Relapse after rigid fixation of mandibular advancement. J Oral Maxillofac Surg 1986;44:698-702
39. Davidson J, Nickerson D, Nickerson P. Zygomatic fractures: comparison of methods of internal fixation. Plast Reconstr Surg 1990;86:25-32
40. Rudderman RH, Mullen RL. Biomechanics of the facial skeleton. Clin Plast Surg 1992;19:11-29
41. Crandall SH, Dahl NC. Introduction to the mechanics of solids. 1st ed. New York: McGraw-Hill, 1959
42. Radin EL, Rose RM, Blaha JD, Litsky AS. Practical biome-chanics for the orthopedic surgeon. 2nd ed. New York: Churchill Livingston, 1992
Reprinted from Annals of Plastic Surgery. Volume 30, Number S, 1993. Published by Little. Brown and Company, Boston, Massachusetts. Copyright © 1993. All rights reserved. No part of this reprint may be reproduced in any form or by any electronic or mechanical means, including information storage and retrieval systems, without the publisher’s written permission.