Restoring and Rejuvenating the Shape of the Eye
The upper and lower lids form the boundary of the eye, which is referred to as the palpebral fissure. The medial canthus and the lateral canthus are the V-like structures where the upper and lower lids meet.
As illustrated below, the youthful palpebral fissure is long and narrow with a slight lateral upward inclination.
This youthful shape may be lost to aging, heredity, paralysis, trauma or surgery.. Typically, this distortion of shape is characterized by rounding of the palpebral fissure as the lateral canthus – or outside edge of the eye – and the lower lid droops.
In most situations, the undesired shape of the palpebral fissure can be improved by repositioning the lateral canthus which at the same time elevates the position of the lower lid. Lateral canthopexy, the surgical repositioning of the lateral canthus is fundamental to altering or restoring the youthful shape of the palpebral fissure.
Two requisites of lateral canthopexy make it technically challenging: symmetry and stability. Suturing of lateral canthal structures to similar points on the inner aspects both lateral orbital rims can be difficult. Stable suture fixation can also be challenging, particularly when previous eyelid surgery has scarred and distorted periorbital tissues.
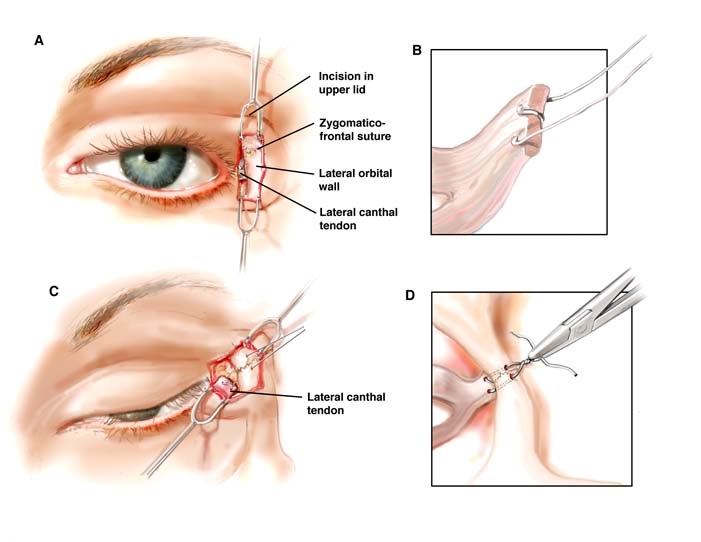
I use the “bridge of bone canthopexy” to reposition the canthus so that they are stable and symmetric. The lateral orbital rim (the bone that borders the side of the eye) and its zygomatic-frontal suture (the anatomic connection of the frontal bone and zygoma bone) are key to stability and symmetry. They are illustrated in Figure A. The lateral canthus is purchased with a suture as shown in Figure B. Figure C shows drill holes made below and above the zygomatic-frontal suture. The suture acts as an anatomic landmark to guide similar and therefore, symmetric positioning of the drill holes on both the right and left orbits. As shown in Figure D, the sutures grasping the lateral canthus are placed through the drill holes and then sutured together over the stable bridge of bone.
Clinical Examples
Clinical examples of the use of the bridge of bone canthopexy are demonstrated below.
A 35-year old woman with Treacher-Collins syndrome underwent augmentation of her coloboma with custom-carved porous polyethylene implants and a bridge of bone canthopexy.
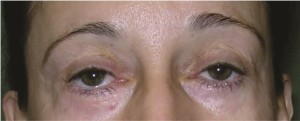
A 50-year old woman had undergone lower lid blepharoplasty in the past. To correct her drooping eyes and restore a more youthful appearance, she underwent subperiosteal midface lift, infraorbital rim augmentation, and lateral canthopexy. (Above) Preoperative frontal view. (Below) One year postoperative view.
A 27 year old woman who not had previous orbital surgery desired upward movement of her lateral canthus.
A 52 year old woman had undergone previous browlift, rhytidectomy and upper and lower lid blepharoplasty. The resulting lower lid retraction had been treated by multiple standard canthopexies, spacer grafts and full thickness skin grafts, but the dry eye symptoms she suffered persisted. Infraorbital rim augmentation, midface lift, and bridge of bone canthopexy resolved her symptoms.
Canthoplasty vs. Canthopexy
The terminology of lateral canthal surgery is confusing given the use of similar terms – canthoplasty and canthopexy – to describe different procedures that yield disparate results.
Lateral canthal or horizontal eyelid shortening procedures – known as canthoplasty – were first developed to treat functional eyelid disorders. By decreasing the surface area of exposed cornea, they ameliorated symptoms of “dry eyes.” They were later adapted to aesthetic surgery as prophylaxis against or to correct undesirable lid position resulting from blepharoplasty (or eyelid) surgery. These lid margin shortening procedures are appropriate treatment when the patient has saggy, excess lower lid skin. They often have negative aesthetic implications, however. Canthoplasty procedures may be effective in elevating the lower lid, but often exaggerate the rounded palpebral fissure shape typical in aging eyes.
On the other hand, a lateral canthopexy repositions the lateral canthus without shortening the lower lid. or altering the lateral commissure – the point where the upper and lower lid meet. Because it moves the intact anatomy of the lateral canthus, it more consistently produces a youthful palpebral fissure shape and lateral canthal angle. By attaching the lateral canthal tendon to the lateral orbital bone, the bridge of bone canthopexy procedures provide sufficient accuracy and stability to correct or protect against undesirable lid position after blepharoplasty.
In bridge of bone canthopexy, a canthal fixation point (the inferior drill hole) creates a measured distance from a fixed anatomic point (the zygomaticofrontal suture) and assures accurate and symmetric placement. Suture fixation over the bridge of bone created by the two drill holes provides maximum stability. When procedures secure the tendon to soft tissue instead of bone, the eye tends to return to its pre-surgery shape over time. Because they maximize accuracy and stability, bridge of bone canthopexy procedures are an excellent choice when a significant correction to canthal position is required.
REFERENCES
Yaremchuk MJ (2003) Restoring palpebral fissure shape after previous lower blepharoplasty. Plast Reconstr Surg;111(1):441-450.
Yaremchuk MJ (2004) Improving periorbital appearance in the morphologically prone. Plast Reconstr Surg;114(4):980-987.
Yaremchuk MJ, Chen Y-C. Bridge of Bone Canthopexy. Aesth Surg J 29:323-329, 2009