The Safe Midface Augmentation with Anatomic Landmarks for the Infraorbital Foramen
Abstract
Introduction: Midface augmentation is routinely used for aesthetic improvement of concave faces while providing a balanced and harmonious contour to the face. It can also be used as an adjunct to orthognathic and reconstructive surgery. An injury to the infraorbital nerve as it exits the infraorbital foramen (IOF) can result in significant morbidity to patients. It presents as a transient or permanent loss of sensation to the midface, nasal sidewall, upper lip, and lower eyelid. The purpose of this study is to identify a safe zone of dissection in the midface for subperiosteal placement of infraorbital, paranasal, malar, and submalar implants while reliably avoiding injury to the infraorbital nerve.
Methods: Given the routine use of transconjuctival and intraoral incisions for access to the midface skeleton, various CT views and 3D models were reviewed in order to identify relevant bony and dental landmarks. Forty-four CT scans of adult hemi-faces were identified. There were 22 males and 22 females in the study, with an average age of 31 years (range from 18 to 45). CT scans were then used for accurate location of the IOF in relationship to our anatomic landmarks.
Results: The location of the IOF correlates most frequently with 2nd premolar on a vertical axis. The average distance between the IOF and the infraorbital rim, the piriform aperture, and the tip of the 2nd premolar cusps is approximately 8.61 mm, 17.43 mm, and 41.81 mm, for males, and 8.25 mm, 15.69 mm, and 37.33 mm, for females, respectively.
Conclusion: A safe zone of dissection for midface augmentation is identified in this study, which does not correlate accurately with previous cadaveric or skull measurements. This may reflect the relatively young age of patients in our study as compared to the findings in published cadaveric measurements. We believe that this zone can greatly assist clinicians in identifying the location of the IOF and avoid injury to the nerve as dissection proceeds from a transconjuctival and an intraoral approach towards the IOF.
 Introduction
 Midface augmentation with alloplastic implants is a common cosmetic procedure with an estimated 8,789 cheek implants procedures in 2009.1 Placement of malar, submalar, or paranasal implants requires intimate knowledge of the anatomy of the midface and the infraorbital foramen. Damage to the infraorbital nerve carries a significant morbidity with numbness to the upper lip, nasal sidewall, lower lid, and midface of the affected side.2 It is difficult to ascertain the exact incident of hypoesthesia following implant placement,3,4 but it is likely that such injuries are underreported in the aesthetic literature. In one study of secondary malar implant surgery, 23% of the patients who sought revision surgery complained of dysesthesias following initial implant placement.5
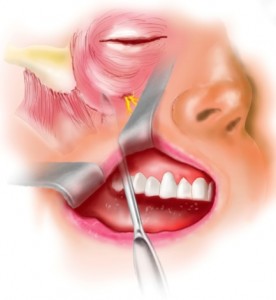
In an effort to prevent these complications, most surgeons rely on experience in order to identify the infraorbital nerve. Moreover, there have been several attempts to identify the infraorbital foramen based on soft tissue landmarks.2,6 The purpose of this study is to define a safe zone of dissection in the subperiosteal plane, while avoiding an injury to the infraorbital nerve based on bony and dental anatomical landmarks. (Fig. 1) Given the routine use of a transconjuctival and an intraoral incisions for our midface augmentation, anatomic landmarks were chosen based on a bidirectional approach.5,7-9
 Materials and Methods
In our study, forty-four spiral CT scans of adult hemi-faces were reviewed (22 males and 22 females). All scans were performed using a standard exposure and patient positioning protocol. The mean age was 31 years with a range from 18 to 45 years. Our exclusion criteria consisted of patients who sustained any midface fracture, bony malformation, or maxillary dental irregularities. Patients younger than 18 years or older than 60 years were excluded as well. Sagittal, axial, and coronal views, as well as 3D reconstruction models were analyzed in order to obtain distance measurements from the IOF.
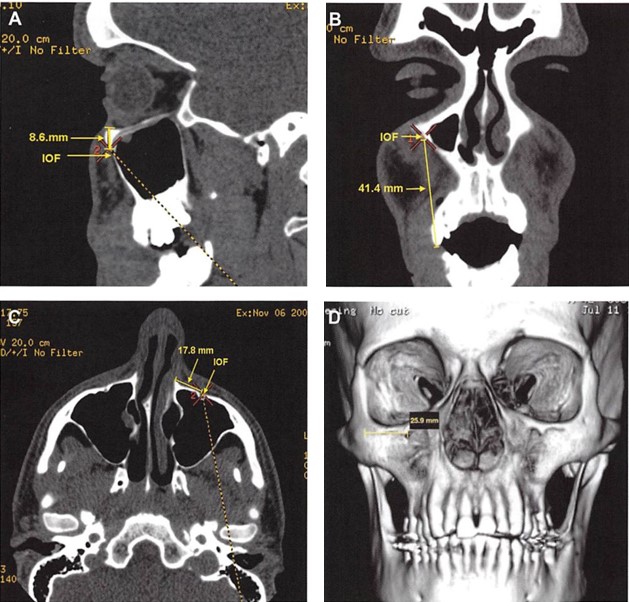
 The following bony and dental landmarks were identified for the IOF: the infraorbital rim, the cusps of the second premolar, and the piriform aperture. The GE Healthcare software “Volume Viewerâ€, version 10.3.67, was utilized in order to obtain our distance measurements. (Fig. 2) A student t test was used to analyze the differences between our male and female groups for each landmark.
Results
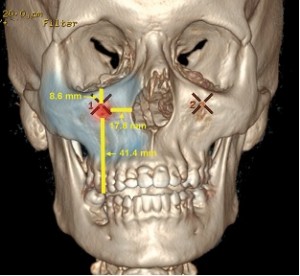
 The location of the IOF correlates most frequently with the 2nd premolar on a vertical axis. The average distance from the IOF to the infraorbital rim, the piriform aperture, and the tip of the 2nd premolar cusps, is approximately 8.61 mm, 17.43 mm, and 41.81 mm, for males, and 8.25 mm, 15.69 mm, and 37.33 mm, for females, respectively. The values of the anatomic landmarks that were measured are listed in Table 1. (Fig. 3)
A statistically significant difference exists between the male and female groups for the distance between the IOF and the tip of the 2nd premolar cusps (P<0.0001), and the distance between the IOF and the PA (P<0.0001). No significant difference was found between the male and the female group for the distance between the IOF and the IOR (P=0.051).
Discussion
 The principal sensory nucleus of the trigeminal nerve lies in the dorsal pons. The trigeminal nerve exists the skull through the foramen rotundum, traverses through the pterygopalatine fossa and enters the orbit through the inferior orbital fissure. It passes through the infraorbital groove and canal in the floor of the orbit. It then exits to the facial skeleton through the infraorbital foramen. At its termination, the nerve lies deep to the levator labii superioris muscle and divides into several branches innervating the nasal sidewall, the lower eyelid, and the upper lip.10
Multiple previous studies have been described to assist clinicians in identifying the location of the IOF for trigeminal nerve blocks, orthognathic surgery, and reconstructive surgery.11-23 In our review of the literature, various soft tissue and bony landmarks were described for the IOF. These include the mid pupil,2 the nasal ala,11 the cheilion (mouth corner),11 the piriform aperture,5,12,16,18,21,24 the inferior orbital rim,11-23 the canine,21 the 1st pre molar,11,25 and the 2nd pre molar tooth.2
We identified inconsistencies in the measurements among various studies, as well as between males and females (Table 2, 3, 4). The majority of these studies were performed on dried skulls, photographs of dried skulls, or cadaveric specimens. Although the average age of these skeletal specimens was not recorded, it is likely that they were of older age. These distances from the IOF to the anatomic landmarks were in most cases smaller than our measurements, perhaps because of the age related changes of the facial skeleton.
The clinical relevance of our study is the young age of our study group, which is usually the common denominator among facial augmentation patients. The importance of facial skeletal aging in relationship to midface augmentation procedures is demonstrated in recent analysis of facial skeletal aging studies.26-28 Several authors illustrated the significant increase in orbital aperture,27 the decrease projection of the midface region,26 and the decrease in facial height27 as a dynamic process of facial bone loss. If all of these variables change with time, the use of measurements from dried cadaveric studies may not be as relevant as the data presented in this study.
Our surgical access to midface augmentation relies mainly on transconjuctival and intraoral approaches.9,29,30 The transconjuctival and buccal incisions are well tolerated by patients, avoid external scarring, and facilitate excellent exposure to the zygomatic and maxillary bones. However, with the absence of proper bony landmarks, it is difficult for the novice surgeon to identify the location of the IOF and prevent injury to the infraorbital nerve. Dissection in the subperiosteal plane can be even more challenging when no soft tissue landmarks could be relied upon. (Fig.1) We recommend the use of high magnification, proper lighting, and excellent hemostasis in order to maximize the visualization of the bony surface anatomy. Moreover, the use of dental and skeletal landmarks can guide the surgeon when operating via small incisions through the lower eyelid and the oral mucosa. The suggested zone of safety is particularly relevant when considering the difference among males and females, as shown in our results (Table 1).
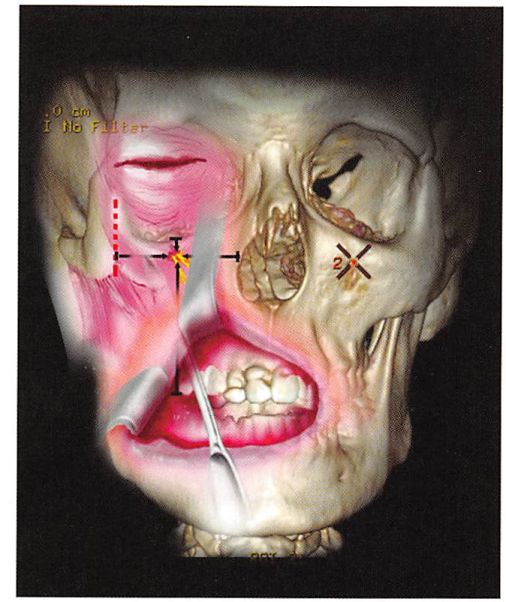
 We also emphasize the need to measure from each anatomic landmark to the outer margin of the IOF in order to avoid entering a danger zone as dissection proceeds inferiorly through a transconjuctival incision or superiorly via a gingivobuccal sulcus incision. (Fig. 4)
 In conclusion, the infraorbital rim, the piriform aperture, and the tip of the 2nd premolar cusps are reliable anatomic landmarks that allow us to define a safe zone of dissection in the midface. We recommend the use of these measurements as they are relevant for both male and female patients, and we hope that they will aid surgeons in avoiding significant morbidity following any midface augmentation procedure.
 FIGURES
 Figure 1. Illustration of an intraoral approach demonstrates the difficulty in identifying the infraorbital foramen in the absence of proper anatomic landmarks.
Figure 2. (A) Sagittal, (B) axial, (C) coronal, and (D) 3-dimensional views show distance measurements from the infraorbital foramen (IOF) to the anatomic landmarks.
 Figure 3. This 3-dimensional model of the skull of a 24-year-old man shows representative measurements from the infraorbital foramen to the anatomic landmarks. Blue shading denotes the safe zone; red shading denotes the danger zone.
Fig. 4. The ability to predict the location of the IOF based bony and dental landmarks.
TABLES
 Table 1. Measurements from the IOF to our anatomic landmarks.
| ÂÂÂ | Parameter | Mean | SD |
| Female | IOF-IOR | 8.25 mm | 0.54 mm |
| IOF-PA | 15,69 mm | 0.76 mm | |
| IOF-2PM | 37.33 mm | 1.58 mm | |
| Male | IOF-IOR | 8.61 mm | 0.64 mm |
| IOF-PA | 17,43 mm | 1.19 mm | |
| IOF-2PM | 41.81 mm | 1.07 mm |
2PM 2nd pre molar tooth, SD standard deviationIOF infraorbital foramen, IOR inferior orbital rim, PA piriform aperture,
Table 2. A comparison of reported measurements from the IOF to the IOR.
| Study | Specimen | IOF – IOR | SD | |
| Hindy & Abdel-Raouf16 | skulls & cadavers | 6.10 mm | N/A | |
| Chrcanovic et al24 | skulls | (f) 6.35 mm
(m) 6.63 mm |
1.67 mm
1.75 mm |
|
| Singh et al.18 | skulls | 6.16 mm | 1.80 mm | |
| Macedo et al.12 | skulls | 6.37 mm | 1.69 mm | |
| Cutright et al17 | cadavers | 6.4 mm
5.8 mm |
0.30 mm
0.30 mm |
|
| Boopathi et al19 | skulls | 6.57 mm | 1.70 mm | |
| Karakas et al.14 | skulls | 6.70 mm | N/A | |
| Elias et al19 | skulls | 6.71 mm | 1.70 mm | |
| Esper et al.18 | skulls | 6.80 mm | N/A | |
| Gupta20 | skulls | 7.0 mm | 1.6 mm | |
| Kazkayasi et al.21 | skulls & x-rays | 7.19 mm | 1.39 mm | |
| Aziz et al.11 | cadavers | 7.8 (f),
8.5 (m) |
1,60 mm
2,2 mm |
|
| Agthong et al22 | skulls | 7.9 | 0,02 mm | |
| Canan et al.13 | cadavers | 8.30 (f),
10.90 (m) |
N/A
N/A |
|
| Chung et al.15 | skull photographs | 8.6 mm | N/A | |
| Apinhasmit et al23 | skulls | 9.23 mm | N/A | |
| Present study | spiral CT scans | (f) 8,25 mm
(m) 8,61 mm |
0,54 mm
0,64 mm |
Table 3. A comparison of reported measurements from the IOF to the PA.IOF infraorbital foramen, IOR inferior orbital rim, SD standard deviation
| Study | Specimen | IOF – PA | SD |
| Hindy & Abdel-Raouf16 | skulls & cadavers | 17.23 mm | N/A |
| Chrcanovic et al24 | skulls | (f) 15.44 mm
(m) 14.37 mm |
1.79 mm
2.04 mm |
| Singh et al.18 | skulls | 15.56 mm | 2.60 mm |
| Macedo et al.12 | skulls | 17.67 mm | 1.95 mm |
| Kazkayasi et al.21 | skulls & x-rays | 14.70 mm | N/A |
| Present study | CTs | (f) 15,69 mm
(m) 17,43 mm
|
0.76 mm
1.19 mm |
IOF infraorbital foramen, PA piriform aperture, SD standard deviation
Table 4. A comparison of reported measurements from the IOF dental anatomical landmarks.
Â
| Study | Specimen | IOF-CT | SD | IOF–1PM | SD | IOF–2PM | SD | |
| Kazkayasi et al.21 | skulls &
x-rays |
33.94mm | 3.15mm | N/A | N/A | N/A | N/A | |
| Brandão et al.25 | skulls | N/A | N/A | 33.4mm | 5.2mm | N/A | N/A | |
| Present study | CTs | N/A | N/A | N/A | N/A | (f) 37,33mm
(m) 41,81mm |
1.58mm
1.07mm |
|
IOF infraorbital foramen, CT canine tooth (lateral process), 1PM 1st premolar tooth (alveolus top),
2PM 2nd premolar (top of the cusps), SD standard deviation
References
- http://plasticsurgery.org/news-and-resources/statistics.html.
- Seckel B. Facial Danger Zones. St Louis: Quality Medical Publishing, Inc.; 1994.
- Yaremchuk MJ. Facial skeletal reconstruction using porous polyethylene implants. Plast Reconstr Surg. May 2003;111(6):1818-1827.
- Maas CS, Merwin GE, Wilson J, Frey MD, Maves MD. Comparison of biomaterials for facial bone augmentation. Arch Otolaryngol Head Neck Surg. May 1990;116(5):551-556.
- Yaremchuk MJ. Secondary malar implant surgery. Plast Reconstr Surg. Feb 2008;121(2):620-628.
- Liu DN, Guo JL, Luo Q, et al. Location of supraorbital foramen/notch and infraorbital foramen with reference to soft- and hard-tissue landmarks. J Craniofac Surg. Jan 2011;22(1):293-296.
- Yaremchuk MJ, Doumit G, Thomas MA. Alloplastic augmentation of the facial skeleton: an occasional adjunct or alternative to orthognathic surgery. Plast Reconstr Surg. May 2011;127(5):2021-2030.
- Yaremchuk MJ, Kahn DM. Periorbital skeletal augmentation to improve blepharoplasty and midfacial results. Plast Reconstr Surg. Dec 2009;124(6):2151-2160.
- Yaremchuk MJ. Making concave faces convex. Aesthetic Plast Surg. May-Jun 2005;29(3):141-147; discussion 148.
- Williams PL. Gray’s Anatomy. 37th ed. New York: Churchill Livingstone; 1989.
- Aziz SR, Marchena JM, Puran A. Anatomic characteristics of the infraorbital foramen: a cadaver study. J Oral Maxillofac Surg. Sep 2000;58(9):992-996.
- Macedo VC, Cabrini RR, Faig-Leite H. Infraorbital foramen location in dry human skulls. Braz J Morphol Sci 2009;26:35-38.
- Canan S, Asim OM, Okan B, Ozek C, Alper M. Anatomic variations of the infraorbital foramen. Ann Plast Surg. Dec 1999;43(6):613-617.
- Karakas P, Bozkir MG, Oguz O. Morphometric measurements from various reference points in the orbit of male Caucasians. Surg Radiol Anat. Feb 2003;24(6):358-362.
- Chung MS, Kim HJ, Kang HS, Chung IH. Locational relationship of the supraorbital notch or foramen and infraorbital and mental foramina in Koreans. Acta Anat (Basel). 1995;154(2):162-166.
- Hindy AM, Abdel-Raouf F. A study of infraorbital foramen, canal and nerve in adult Egyptians. Egypt Dent J. Oct 1993;39(4):573-580.
- Cutright B, Quillopa N, Schubert W. An anthropometric analysis of the key foramina for maxillofacial surgery. J Oral Maxillofac Surg. Mar 2003;61(3):354-357.
- Singh R. Morphometric analysis of infraorbital foramen in Indian dry skulls. Anat Cell Biol. Mar 2011;44(1):79-83.
- Boopathi S, Chakravarthy Marx S, Dhalapathy SL, Anupa S. Anthropometric analysis of the infraorbital foramen in a South Indian population. Singapore Med J. Sep 2010;51(9):730-735.
- Gupta T. Localization of important facial foramina encountered in maxillo-facial surgery. Clin Anat. Oct 2008;21(7):633-640.
- Kazkayasi M, Ergin A, Ersoy M, Bengi O, Tekdemir I, Elhan A. Certain anatomical relations and the precise morphometry of the infraorbital foramen–canal and groove: an anatomical and cephalometric study. Laryngoscope. Apr 2001;111(4 Pt 1):609-614.
- Agthong S, Huanmanop T, Chentanez V. Anatomical variations of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg. Jun 2005;63(6):800-804.
- Apinhasmit W, Chompoopong S, Methathrathip D, Sansuk R, Phetphunphiphat W. Supraorbital Notch/Foramen, Infraorbital Foramen and Mental Foramen in Thais: anthropometric measurements and surgical relevance. J Med Assoc Thai. May 2006;89(5):675-682.
- Chrcanovic BR, Abreu MH, Custodio AL. A morphometric analysis of supraorbital and infraorbital foramina relative to surgical landmarks. Surg Radiol Anat. May 2011;33(4):329-335.
- Brandão FH, Machado MRC, Aquino JEP, Coelho RGj, Pereira SH, Fabi RP. The Foramen and Infraorbital Nerve relating to the Surgery for External Access to the Maxillary Sinus (CALDWELL-LUC). 2008;12 (3).
- Coleman SR, Grover R. The anatomy of the aging face: volume loss and changes in 3-dimensional topography. Aesthet Surg J. Jan-Feb 2006;26(1S):S4-9.
- Shaw RB, Jr., Katzel EB, Koltz PF, et al. Aging of the facial skeleton: aesthetic implications and rejuvenation strategies. Plast Reconstr Surg. Jan 2011;127(1):374-383.
- Bartlett SP, Grossman R, Whitaker LA. Age-related changes of the craniofacial skeleton: an anthropometric and histologic analysis. Plast Reconstr Surg. Oct 1992;90(4):592-600.
- Terino EO. Alloplastic midface augmentation. Aesthet Surg J. Sep-Oct 2005;25(5):512-520.
- Binder WJ. Facial rejuvenation and volumization using implants. Facial Plast Surg. Feb 2011;27(1):86-97.
Â

Leave Comments
You must be logged in to post a comment.